Labs and Lytes 037
Author: Dr Craig Johnston
Reviewers: A/Prof Chris Nickson
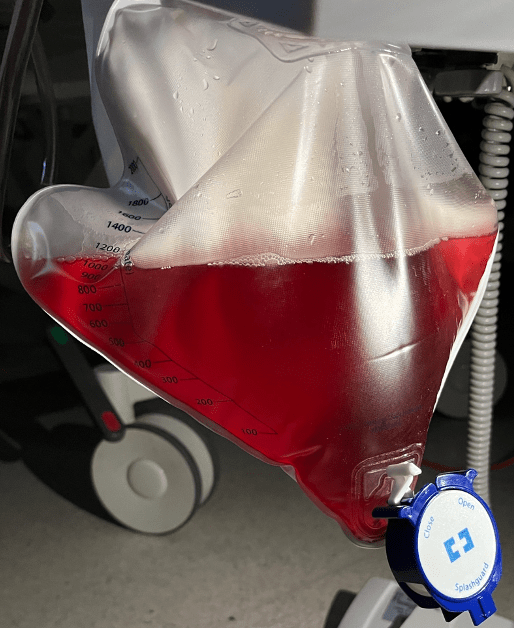
On your nightshift, the bedside nurse asks you to review a 65-year-old female with red urine in her indwelling urinary catheter bag. She has just been admitted to ICU following a house fire where she was trapped and has been intubated after sustaining an inhalational injury. There was no other traumatic injury sustained and a urine dip is negative for haemoglobin.
Q1. What is the likely reason for her discoloured urine?
Hydroxocobalamin has been administered.
A red discolouration to the skin and mucous membranes may also be noted in addition to the urine1,2.
Q2. Why was the agent (identified in Q1) administered?
This patient had suspected cyanide toxicity.
The indications1,4 for hydroxocobalamin in suspected cyanide toxicity include:
- Altered mental status
- Seizures
- Hypotension
- Lactic acidosis
Q3. How does this underlying condition (identified in Q2) manifest clinically?
Cyanide toxicity1,3 results from cyanide binding to the ferric ion (Fe3+) of cytochrome oxidase, inhibiting oxidative phosphorylation in mitochondria.
Early clinical features include
- Nausea and vomiting
- Headache
- Tachycardia and tachypnoea
- Agitation
- Seizures
Late clinical features include
- Hypotension and bradycardia
- Confusion
- Tetany
- Respiratory depression
- Coma
Investigations usually reveal
- hyperlactataemia and high anion gap acidosis.
- high venous O2 saturation, with a low arterial-venous oxygen difference (i.e. a low O2 extraction ratio as mitochrondria are unable to utilise oxygen).
Q4. What is the mechanism of action for the agent identified in Q1?
Hydroxocobalamin is a vitamin B12 precursor1,4,5.
In high doses it chelates cyanide, forming cyanocobalamin which is non-toxic and excreted in urine
Aerobic metabolism can then resume normally.
Hydroxocobalamin is available as a “Cyanokit®” containing 2 vials of 2.5g hydroxocobalamin as a powder, and 2 vials of 100ml 0.9% NaCl for reconstitution.
To administer:
- Reconstitute one vial (2.5g) in 100ml of 0.9% NaCl, and give over 15 mins
- Repeat with the second vial
- This should be sufficient to bind 100mg of cyanide (but often quantity is unclear with inhalational injury)
- If patient is in cardiac arrest, give 5g as an IV push.
Note that this dose is huge in comparison to the dose given for Vitamin B12 deficiency (250 – 1000mcg per IM injection).
Hydroxocobalamin has a low side effect profile, in that if it is given to a patient without cyanide poisoning, there is low risk of an adverse outcome.
Q5. What commonly used ICU drug can also cause the underlying condition identified in Q2?
Sodium nitroprusside.
SNP contains 5 cyanide groups and one nitric oxide group attached to a central iron molecule covalently bonded to Na.
When SNP reacts with oxyhaemoglobin in red blood cells, it releases nitric oxide (causing arterial and venous vasodilation and reducing MAP), and also 5 cyanide ions.
At high dose this can cause cyanide toxicity.
References
- Murray L, Little M, Pascu O, Hoggett K. Toxicology Handbook, 3rd Edition. Australia: Elsevier Australia; 2016
- Cescon D, Juurlink D. Discoloration of skin and urine after treatment with hydroxocobalamin for cyanide poisoning. CMAJ 2009; 180(2): 251 [article]
- Nickson CP. Cyanide Poisoning. LITFL CCC. Accessed 22 Feb 2022. Available at URL: https://litfl.com/cyanide-poisoning-ccc/
- Nickson CP. Hydroxocobalamin. LITFL. Accessed 23 Feb 2022. Available at URL: https://litfl.com/hydroxocobalamin/
- Therapeutic Goods Administration: Product and Consumer Information. Hydroxocobalamin. Accessed 23 Feb 2022. Available at URL: https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-07721-3&d=20220223172310101
All case-based scenarios on INTENSIVE are fictional. They may include realistic non-identifiable clinical data and are derived from learning points taken from clinical practice. Clinical details are not those of any particular person; they are created to add educational value to the scenarios.