Everything ECMO 038
Author: Dr Sandra Emily Stoll
Reviewer: A/Prof Chris Nickson
A 52-year-old male presents to the hospital after resuscitation for out-of-hospital cardiac arrest (OOHCA) due to ventricular fibrillation caused by a myocardial infarction. As he remained haemodynamically unstable, despite immediate bystander cardiopulmonary resuscitation (CPR) and return of spontaneous circulation (ROSC) after 10 minutes of low flow time, the decision was made to initiate veno-arterial extracorporeal membrane oxygenation (VA-ECMO) support.
After ECMO initiation the fresh gas flow delivered to the ECMO membrane was set at a blender oxygen fraction (FbO2) 1.0 and his ventilator fraction of inspired oxygen (FiO2) was set at 100%. An arterial blood gas (ABG) analysis was obtained from his right radial artery and revealed an arterial oxygen partial pressure (PaO2)of 420 mmHg.
The treating nurse raises whether this “hyperoxia” is harmful and what the oxygen targets should be for this patient.
Q1: What is the definition of hyperoxia?
Hyperoxia occurs when arterial partial pressure of oxygen (PaO2) exceeds the normal range (60-100 mmHg) that occurs when breathing air at one atmospheric pressure.
There are currently no consensus definitions for hyperoxia. Some references define moderate hyperoxia as an PaO2-level of 101-299 mmHg and severe hyperoxia ≥300 mmHg.(1) Most literature on the impact of oxygen on the outcome of cardiac arrest concern this latter category.
Q2: How does hyperoxia occur?
Hyperoxia can occur for different reasons, and can be normobaric or hyperbaric:
Normobaric hyperoxia:
Normobaric hyperoxia occurs at one atmospheric pressure due to an increased inspired fraction of oxygen FiO2 (FiO2 1.0) when breathing via the lungs, or due to oxygenation from the fresh gas flow to the membrane (FbO2) during ECMO support. The risk of hyperoxia with VA-ECMO is usually high as FbO2 in VA-ECMO is traditionally set at 1.0 to avoid cardiac or cerebral hypoxia (see What is different about hypoxia on VA-ECMO?).
Hyperbaric hyperoxia:
Hyperoxia is a result of supranormal atmospheric pressure (e.g. hyperbaric therapy) with or without an increased FiO2. FiO2 could be even lower than the normal FiO2 of 0.21 and still result in a higher PaO2 than normal due if the ambient pressure is increased high enough.
Q3: Why can hyperoxia be harmful?
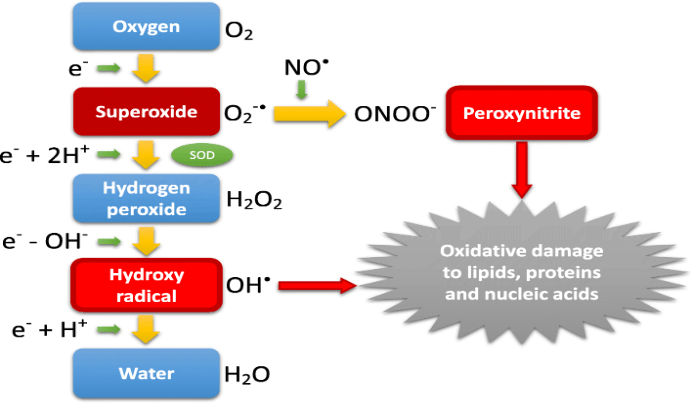
Hyperoxia can lead to oxygen toxicity caused by the harmful effects of breathing molecular oxygen at elevated partial pressures. This is mediated by increased amounts of reactive oxygen species (ROS).
ROS are chemically reactive oxygen containing molecules which can stimulate proinflammatory responses and damage lipids, proteins, and nucleic acids in surrounding biological tissues. Normally the human body naturally produces antioxidants against ROS, but antioxidants can be overwhelmed and depleted by recurrent high amounts of ROS. This leads to oxidation of tissues and organ toxicity syndrome / oxygen intoxication.
Q4: Is hyperoxia harmful due to dose, timing, or duration of exposure?
It is not certain if hyperoxia is harmful due to the timing of exposure, the severity of exposure, duration of exposure or a mix of these factors.
In fact, there is no clear threshold associated with a risk of harm (see also Q6). The risk of harm probably increases depending on the patient’s individual oxygen demand, organ vulnerability (neonates are more vulnerable than adults), individual antioxidant capacity, dosage of oxygen exposure, duration of oxygen exposure, timing of oxygen exposure (e.g. pre or post cardiac arrest) and multiple other factors.
Q5: What effect does normobaric hyperoxia have on the human body?
The following list (modified from DerangedPhysiology.com’s “Physiological effects of hyperoxia”) presents effects of oxygen toxicity in different organ systems due to normobaric hyperoxia.
| Tissue | Effects |
| Airway (FiO2 increased) | Mucositis, Tracheitis, Bronchitis |
| Lung (FiO2 increased) | Absorption atelectasis Alveolar toxicity (Lorraine Smith effect) Pulmonary vasodilatation / pulmonary edema Disturbance of V/Q match Pulmonary capillary leak Denitrogenation of gas cavities (e.g. pneumothorax) |
| Lung (FiO2 or FbO2 increased) | Respiratory drive decreased |
| Gas carriage | Reverse Haldane effect: Increased release of CO2 from hemoglobin Increased clearance of CO2 |
| Cardiovascular system | (Coronary) vasoconstriction due to accelerated rate of oxidative degradation of nitric oxide in the endothelium Increased systemic vascular resistance (SVR) Increased cardiac work, decreased cardiac output |
| Cerebral circulation | Decreased cerebral blood flow Cerebral vasoconstriction |
| Metabolic | Increased production of free radicals |
| Immune system | Immunosuppressant effect Increases amount of circulating inflammatory cytokines |
| Infectious disease | Impairment of reproduction of anaerobes |
| Bone marrow | Bone marrow depression Impairment of Erythropoiesis |
| Ocular toxicity (in neonates) | Retinopathy / Cataract |
Harm associated with hyperoxia has been found in studies of several subgroups of intensive care patients(3, 4), including patients suffering from sepsis (5, 6), stroke(7), traumatic brain injury(8), myocardial infarction (9, 10) and cardiac arrest. (1, 5, 11-13)
Post CA patients are thought to be especially vulnerable as ischemia-reperfusion injury can be aggravated by hyperoxia. This may have contributed to the findings of the ICU-ROX trial, where patients with ischemic hypoxic encephalopathy showed better outcomes when managed with a conservative oxygen approach compared with a liberal oxygen approach.(14) Large, prospective multicenter trials such as the MEGA-ROX-trial will focus more on these vulnerable subgroups of ICU patients, as definitive evidence is still lacking.
Q6: How common is hyperoxia in CA and does hyperoxia have an effect on mortality after CA?
Hypoxia and severe hyperoxia have both been proposed to have an association with mortality, as represented by a U-shaped curve (see figure 2, sourced from Pastene at al. (15)). However, the thresholds for harmful oxygen levels remain unclear.
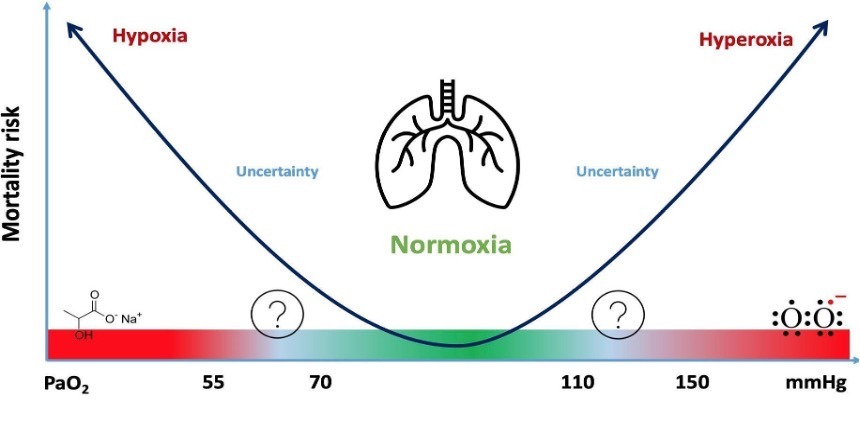
Hyperoxia is a common phenomenon in CA-patients and is thought to be associated with an increased mortality.(16, 17) A retrospective, multicenter study by Kilgannon et al. 2010 including 6326 CA-patients showed that hyperoxia was present in 18%.(11) In patients treated with VA-ECMO for CA this incidence is even higher, as a retrospective study conducted at the Alfred hospital recently showed: hyperoxia occurred in 74.7% of CA patients treated with ECMO-CPR (VA-ECMO) versus 16.7% in CA patients managed with conventional CPR.(18) Furthermore this study revealed, that hyperoxia was associated with a 2.52-fold increased risk of 30-day mortality irrespective of whether patients were resuscitated by conventional CPR or by ECMO-CPR.
Several large, retrospective studies found an association of hyperoxia with a higher mortality (11, 12, 19), but others did not reveal this association, in CA patients.(20, 21) Evidence so far is conflicting, and evidence from large prospective, randomized controlled trials is currently lacking.
Q7: What should be the target oxygen levels for patients post CA?
At present, international societies as the Australian and New Zealand Committee on Resuscitation (ANZCOR)(22) and the American Heart Association (AHA) recommend the application of 100% oxygen during resuscitation of CA.(23) After establishment of ROSC, when reliable monitoring of oxygen saturation (SpO2 or ABGs) is continuously available, the AHA recommendations for CA patients include the titration of inspired oxygen by reducing FiO2 to achieve a target saturation between 94 – 98% or a PaO2 of 60-100mmHg.
The HOT OR NOT-trial by Young et al. (2014) studied oxygen targets of CA patients in the pre-hospital setting and found that conservative oxygen titration was not feasible in the pre-hospital setting and should be postponed to hospital admission.(24) The EXACT-trial, a large multi-center, randomized, single-blind, parallel trial, has been underway since 2019 and is currently collecting outcome data after CA in patients administered either conservative (SpO2 94-98%) or liberal (SpO2 98-100%) oxygen titration in the prehospital setting. (25) Results are still awaited.
In patients treated with VA-ECMO for CA, hyperoxia should be monitored with frequent arterial blood gases. All ABGs should be taken from the right arm to avoid the risk of differential hypoxaemia during VA-ECMO. In VA-ECMO, PaO2 is mainly titrated by FbO2. In VA-ECMO the fraction of oxygen in the fresh gas delivered to the membrane (FbO2) traditionally was set at 1.0 (100% O2) resulting in high PaO2-levels. In recent years, some ECMO-centres worldwide start titrating FbO2 to patients´oxygen demand. The BLENDER trial (NCT03841084), which also commenced in 2019, aims to determine whether a conservative or liberal oxygen strategy improves outcomes in patients treated with VA-ECMO. This will be the first randomized controlled trial data addressing this question.
References
- Munshi L, Kiss A, Cypel M, Keshavjee S, Ferguson ND, Fan E. Oxygen Thresholds and Mortality During Extracorporeal Life Support in Adult Patients. Crit Care Med. 2017;45(12):1997-2005. [pubmed]
- Nakane M. Biological effects of the oxygen molecule in critically ill patients. J Intensive Care. 2020;8(1):95. [pubmed]
- Martin J, Mazer-Amirshahi M, Pourmand A. The Impact of Hyperoxia in the Critically Ill Patient: A Review of the Literature. Respir Care. 2020;65(8):1202-10. [pubmed]
- Helmerhorst HJ, Roos-Blom MJ, van Westerloo DJ, de Jonge E. Association Between Arterial Hyperoxia and Outcome in Subsets of Critical Illness: A Systematic Review, Meta-Analysis, and Meta-Regression of Cohort Studies. Crit Care Med. 2015;43(7):1508-19. [pubmed]
- Halter M, Jouffroy R, Saade A, Philippe P, Carli P, Vivien B. Association between hyperoxemia and mortality in patients treated by eCPR after out-of-hospital cardiac arrest. Am J Emerg Med. 2019. [pubmed]
- Demiselle J, Wepler M, Hartmann C, Radermacher P, Schortgen F, Meziani F, et al. Hyperoxia toxicity in septic shock patients according to the Sepsis-3 criteria: a post hoc analysis of the HYPER2S trial. Ann Intensive Care. 2018;8(1):90. [article]
- Rincon F, Kang J, Maltenfort M, Vibbert M, Urtecho J, Athar MK, et al. Association between hyperoxia and mortality after stroke: a multicenter cohort study. Crit Care Med. 2014;42(2):387-96. [pubmed]
- Brenner M, Stein D, Hu P, Kufera J, Wooford M, Scalea T. Association between early hyperoxia and worse outcomes after traumatic brain injury. Arch Surg. 2012;147(11):1042-6. [pubmed]
- Stub D, Smith K, Bernard S, Bray JE, Stephenson M, Cameron P, et al. A randomized controlled trial of oxygen therapy in acute myocardial infarction Air Verses Oxygen In myocarDial infarction study (AVOID Study). Am Heart J. 2012;163(3):339-45 e1. [pubmed]
- Ross P, Miller C, Sheldrake J, McGuiness W, Udy A, Burrell A. Hyperoxia in patients with cardiogenic shock after myocardial infarction supported with venoarterial extracorporeal membrane oxygenation. Aust Crit Care. 2020. [pubmed]
- Kilgannon JH, Jones AE, Shapiro NI, Angelos MG, Milcarek B, Hunter K, et al. Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA. 2010;303(21):2165-71. [article]
- Kilgannon JH, Jones AE, Parrillo JE, Dellinger RP, Milcarek B, Hunter K, et al. Relationship between supranormal oxygen tension and outcome after resuscitation from cardiac arrest. Circulation. 2011;123(23):2717-22. [pubmed]
- Vincent JL, Taccone FS, He X. Harmful Effects of Hyperoxia in Postcardiac Arrest, Sepsis, Traumatic Brain Injury, or Stroke: The Importance of Individualized Oxygen Therapy in Critically Ill Patients. Can Respir J. 2017;2017:2834956. [article]
- Investigators I-R, the A, New Zealand Intensive Care Society Clinical Trials G, Mackle D, Bellomo R, Bailey M, et al. Conservative Oxygen Therapy during Mechanical Ventilation in the ICU. N Engl J Med. 2020;382(11):989-98. [pubmed]
- Pastene B. et al; Oxygen: Too much is bad. ICU Management & Practice, Volume 21 – Issue 3, 2021. [article]
- Wang CH, Chang WT, Huang CH, Tsai MS, Yu PH, Wang AY, et al. The effect of hyperoxia on survival following adult cardiac arrest: a systematic review and meta-analysis of observational studies. Resuscitation. 2014;85(9):1142-8. [pubmed]
- Patel JK, Kataya A, Parikh PB. Association between intra- and post-arrest hyperoxia on mortality in adults with cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2018;127:83-8. [pubmed]
- Stoll SE, Paul E, Pilcher D, Udy A, Burrell A. Hyperoxia and mortality in conventional versus extracorporeal cardiopulmonary resuscitation. J Crit Care. 2022;69:154001. [pubmed]
- Janz DR, Hollenbeck RD, Pollock JS, McPherson JA, Rice TW. Hyperoxia is associated with increased mortality in patients treated with mild therapeutic hypothermia after sudden cardiac arrest. Crit Care Med. 2012;40(12):3135-9. [article]
- Ihle JF, Bernard S, Bailey MJ, Pilcher DV, Smith K, Scheinkestel CD. Hyperoxia in the intensive care unit and outcome after out-of-hospital ventricular fibrillation cardiac arrest. Crit Care Resusc. 2013;15(3):186-90. [pubmed]
- Bellomo R, Bailey M, Eastwood GM, Nichol A, Pilcher D, Hart GK, et al. Arterial hyperoxia and in-hospital mortality after resuscitation from cardiac arrest. Crit Care. 2011;15(2):R90. [pubmed]
- ANZCOR. Guideline 11.6.1 – Targeted Oxygen Therapy in Adult Advanced Life Support; . 2016. [article]
- Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, et al. Part 8: Post-Cardiac Arrest Care: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S465-82. [pubmed]
- Young P, Bailey M, Bellomo R, Bernard S, Dicker B, Freebairn R, et al. HyperOxic Therapy OR NormOxic Therapy after out-of-hospital cardiac arrest (HOT OR NOT): a randomised controlled feasibility trial. Resuscitation. 2014;85(12):1686-91. [pubmed]
- Bray JE, Smith K, Hein C, Finn J, Stephenson M, Cameron P, et al. The EXACT protocol: A multi-centre, single-blind, randomised, parallel-group, controlled trial to determine whether early oxygen titration improves survival to hospital discharge in adult OHCA patients. Resuscitation. 2019;139:208-13. [pubmed]