Labs and Lytes 026
Author: Virginia Newcombe
Reviewer: Chris Nickson
You are the ICU registrar on call and asked to attend the Emergency Department to assist with a hypotensive patient who was GCS 15.
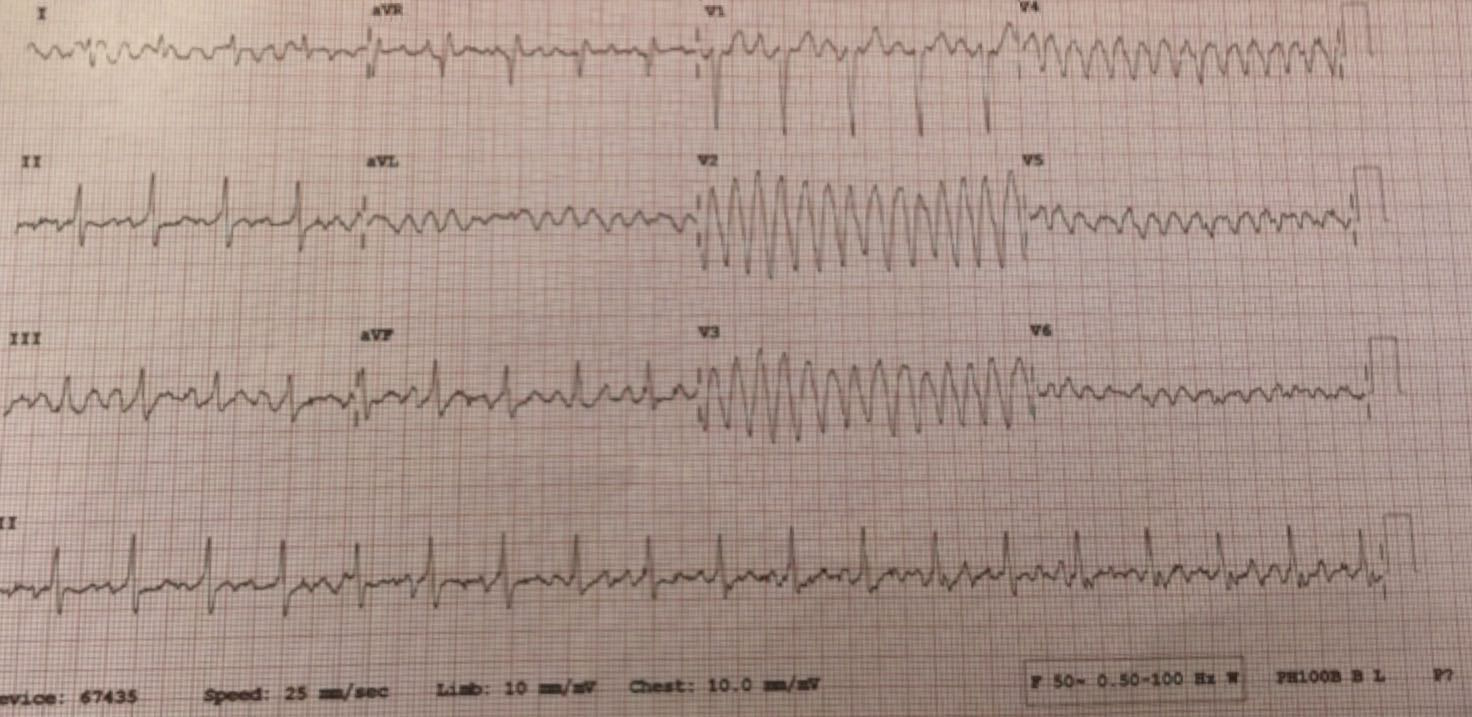
On arrival to resus you are shown the following ECG:
Q1. Describe the ECG findings.
The rhythm strip (Lead II) shows a rate of approximately 150 bpm. While it appears regular the baseline is jagged, which may suggest flutter. The anteroseptal (V2-4) and lateral leads (V5-6) show a broad complex tachycardia consistent with a polymorphic VT.
Q2. What is the cause of these ECG findings?
While tempting to assume that the lateral leads are secondary to artefacts – for example a loose lead, tremor, etc – the normal rhythm strip and the pattern makes it unlikely.
This patient has had a heterotopic transplant and has presented with one of his hearts in VT and the other in a sinus rhythm. Before the advent of ventricular assist devices (or VA ECMO) heterotopic cardiac transplantation was performed when the donor heart did provide sufficient cardiac function on its own. In this procedure the patient’s own heart is remians in situ and the new heart is positioned so that the chambers and blood vessels of both hearts are connected to form what is effectively a “double heart.” In particular, it may be performed in patients with refractory pulmonary hypertension. For these patients, orthotopic transplantation without a VAD or other assistance is at high risk of the donor heart failing due to elevated right heart pressures. Heterotopic transplantation may also be used when there is a significant mismatch between the patient size and heart size. In this case if the donor heart is too small then the recipient heart may take on the “assist device” role, and so help supporting the circulation during the initial adaptation.

This image is taken from http://med.stanford.edu/news/all-news/2004/two-hearts-are-better-than-one-for-toddler-who-undergoes-historic-operation.html Image Credit: Abdulaziz Alkhaldi, MD – click image for source.
Of course an alternative explanation for this ECG is that there is a Gallifreyan in your resus bay!
Q3. How would you manage this patient?
Manage as for VT in patients with one heart but with some key differences.
General Principles
- Ensure potassium levels are adequate
- Consider magnesium supplementation
- Consider anti-arrythmics including amiodarone
- Treat any precipitants
- Consider DC cardioversion if above not successful or evidence of compromise
When performing an electrical cardioversion in patients with a heterotopic transplant is it important to ensure that the synchronisation is to the R wave of “normally” beating heart otherwise ventricular fibrillation may be induced. The pads should be placed over the heart that you are trying to deliver the shock to.
To decide which heart is in VT is can be useful to perform two ECGs; a traditional left sided one and a complete right sided ECG, as well as simply palpating the chest or using echocardiography.
Below is the right sided ECG taken at the same time as the ECG in Question 1. In this ECG VT can only be convincingly seen in R1 further adding evidence that it is the native heart which is in VT.
Q4. What might you see on a ‘normal’ ECG in these types of patients?
It is common to see two electrical complexes competing with each other.
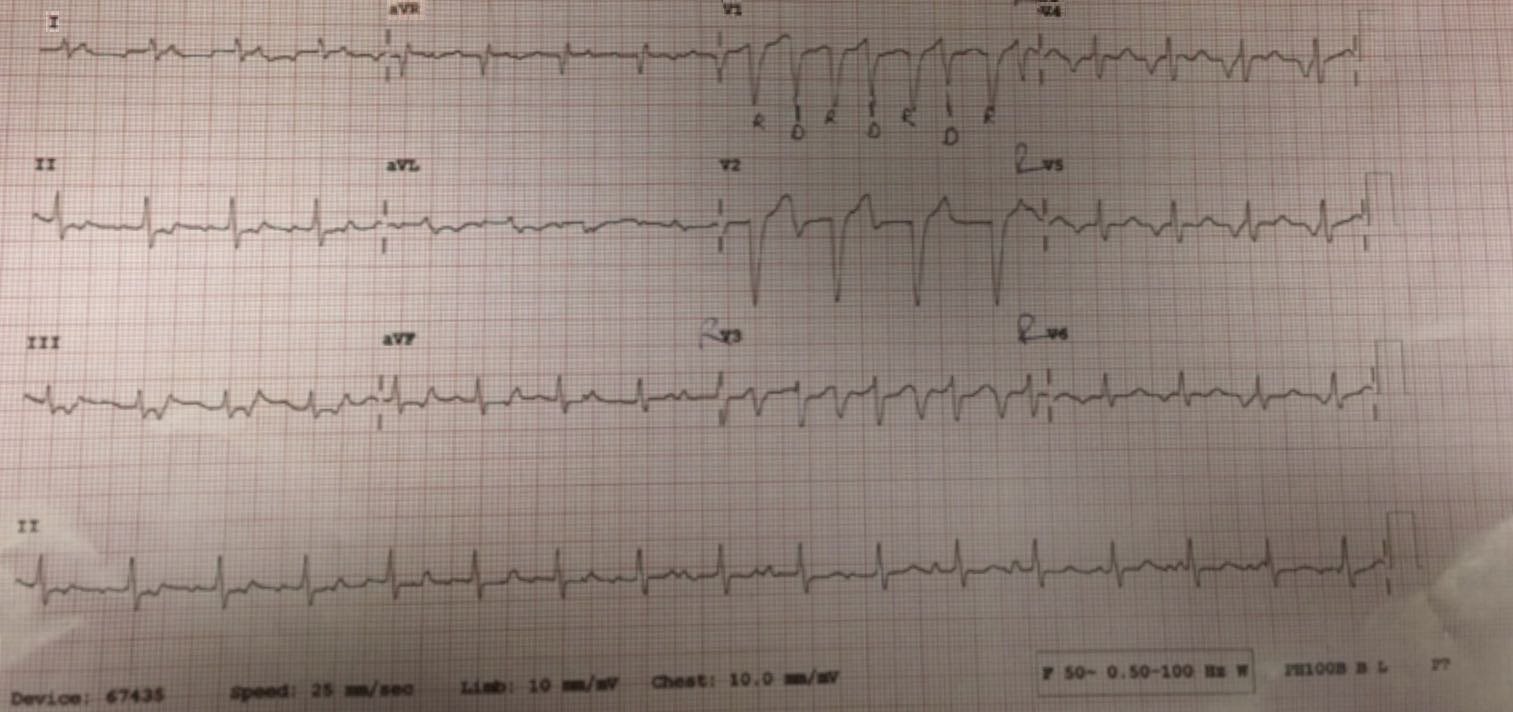
Below are the left and right sided ECGs for the patient in this scenario post DC cardioversion. The donor heart is in a rhythm of approximately 100bpm and the recipient heart is in AF with a ventricular rate of approximately 100bpm. The donor and recipient beats are labeled on the right sided ECG as R and D respectively.
Left sided ECG:
Right sided ECG:
All case-based scenarios on INTENSIVE are fictional. They may include realistic non-identifiable clinical data and are derived from learning points taken from clinical practice. Clinical details are not those of any particular person; they are created to add educational value to the scenarios.


What a great case, got the A flutter but could not get my mind around the VT bit, thought it would be artefact??? Thank you
Pingback: LITFL Review 224 • LITFL Medical Blog • FOAMed Review