Labs and Lytes 032
Author: Xiuxian Pham
Peer Reviewer: Chris Nickson
A 60-year-old man with diffuse large B-cell lymphoma is admitted to intensive care with multi-organ failure. He is day 13 post conditioning regimen with LACE (lomustine, cytarabine, cyclophosphamide and etoposide) and an autologous stem cell transplant. His primary active issue is sepsis but amongst his other active issues including abnormal liver function tests.
| LFTs | On admission to hospital | On admission to ICU | Reference |
|---|---|---|---|
| Total protein | 61 | 56 | 60-80 |
| Albumin | 36 | 15 | 33-46 |
| Globulin | 25 | 41 | 24-39 |
| Bilirubin | 20 | 78 | <21 |
| ALT | 70 | 69 | <40 |
| GGT | 97 | 196 | <62 |
| ALP | 65 | 58 | 30-110 |
The patient is noted to be jaundiced, with a distended abdomen, mild hepatomegaly and has been gaining weight in the lead up to his ICU admission.
Q1. What specific diagnosis should you consider in this patient given his history?
Sinusoidal obstruction syndrome (SOS), also known as veno-occlusive disease (VOD)
This condition is important to identify given severe forms can lead to multi-organ failure and death. It typically occurs <3 weeks after haematopoietic stem cell transplant and – like Budd-Chiari syndrome – is characterised by the triad of:
- Tender hepatomegaly
- Jaundice
- Ascites (or weight gain/ fluid retention)
Other causes of SOS include: some monoclonal antibodies (e.g. gemtuzumab, inotuzumab), alkaloid toxins, high dose liver radiotherapy, and liver transplantation
Q2. What is the underlying pathogenesis?
Pathogenesis:
- Injury to sinusoidal endothelial cells and hepatocytes in zone 3
- Leads to gaps in sinusoidal barrier, allowing red blood cells, white blood cells and cellular debris to pass through gaps
- Progressive venular occlusion results in post-sinusoidal portal hypertension
Q3. What are the risk factors for this diagnosis?
Risk factors include:
- Pre-existing liver disease
- Intensity of conditioning therapy (higher with cyclophosphamide)
- Allogeneic > autologous grafts
- Age (higher in children)
- Poor baseline performance status
Q4. What investigations would you organise next and how would you confirm the diagnosis?
Useful investigations include:
- Coagulation studies: to assess liver synthetic function
- FBE: thrombocytopaenia from hypersplenism due to portal hypertension
- UEC: renal failure occurs in severe manifestations
- Imaging: may be abnormal but not diagnostic for SOS; however, utilised to rule out other differentials for cholestatic LFTs
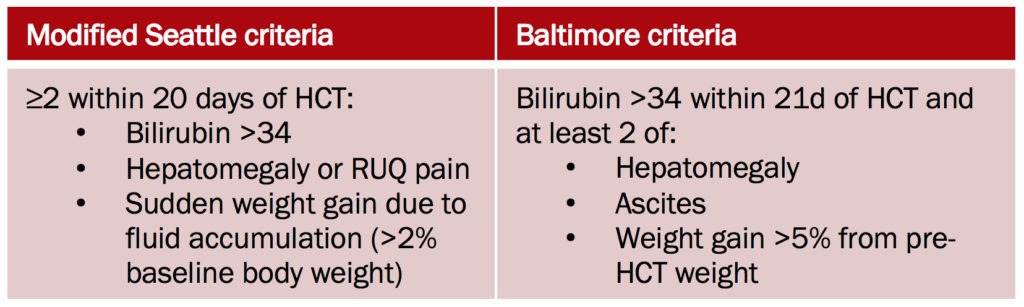
However, SOS is essentially a clinical diagnosis. Both the modified Seattle criteria and the Baltimore criteria includes raised bilirubin, hepatomegaly, weight gain that occurs within 3 weeks of haematopoietic stem cell transplant:
Q5. What is the treatment?
Treatment consists of:
- Supportive care
- If severe: defibrotide for 21-60 days until bilirubin normalised
Options for prevention are:
- ursodeoxycholic acid, or
- low-dose heparin
References
- Dignan FL, Wynn RF, Hadzic N, et al. BCSH/BSBMT guideline: diagnosis and management of veno-occlusive disease (sinusoidal obstruction syndrome) following haematopoietic stem cell transplantation. Br J Haematol. 2013;163(4):444-57. [article]
- Fulgenzi A, Ferrero ME. Defibrotide in the treatment of hepatic veno-occlusive disease. Hepat Med. 2016;8:105-113. [article]
- Valla DC, Cazals-hatem D. Sinusoidal obstruction syndrome. Clin Res Hepatol Gastroenterol. 2016;40(4):378-85. [article]
All case-based scenarios on INTENSIVE are fictional. They may include realistic non-identifiable clinical data and are derived from learning points taken from clinical practice. Clinical details are not those of any particular person; they are created to add educational value to the scenarios.