Everything ECMO 044: Persistent and refractory hypoxaemia on VV-ECMO – Part 2
Author: Dr Alastair Brown
Peer reviewers: Dr Aidan Burrell, Dr Arne Diehl, A/Prof Chris Nickson
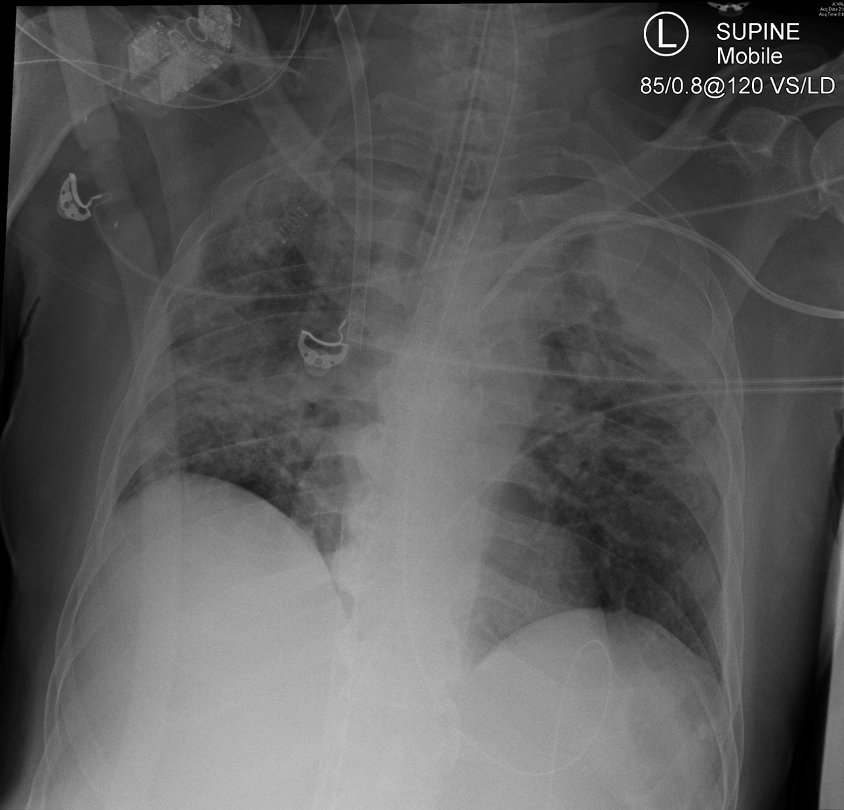
A 54-year-old man with psittacosis pneumonia was commenced on femoro-jugular VV ECMO and was transferred to your centre for ongoing management. Despite increasing ECMO blood flow to 6 L/min it has not been possible to achieve an Sp02 > 88%. The access saturation (pre-oxygenator SO2) on the HLS ECMO console is 95%. His chest radiograph is shown below:
Q1. What is the likely cause of the issue?
Re-circulation.
Re-circulation on VV-ECMO may can occur when access and return cannula inlets are placed too close together. Blood returned to the patient re-circulates via the access cannula back in the ECMO circuit, rather than moving through the pulmonary circulation1.
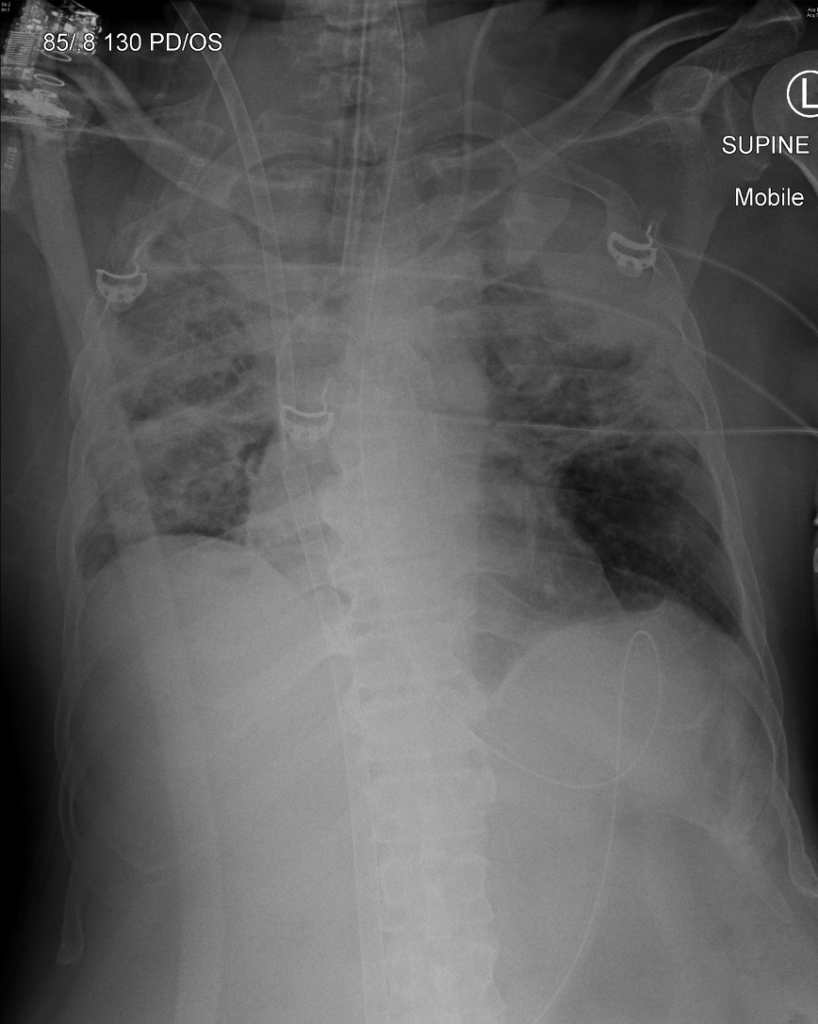
Note that the femoral access cannula and the jugular return cannula appear to overlap in Figure 1, making localisation of their tips difficult. Ideally, the tip of the return cannula should be positioned at least 9 cm distant from the proximal hole of a multistage access cannula (distal holes contribute much less to drainage). Remember that the distal 4cm of the ECMO cannula is radio-lucent making it invisible on radiographs. Recirculation is more common in tall patients when cannulas are placed lower in the inferior vena cava (IVC) (see Figure 2, below).
Q2. What determines the extent of this phenomenon?
The extent of recirculation is a function of three variables:
- pump speed
- cannula configuration
- patient cardiac output
Q2. What signs suggest it is clinically significant?
Signs of clinically significant recirculation include:
- Poor colour differential between access and return limb of circuit. Both will be bright red in colour.
- High oxygen saturation in access limb (e.g. pre-oxygenator SO2 >80%)
- No improvement in oxygen saturation with increase in ECMO blood flow.
Q3. How can this be managed?
Possible solutions:
- Adjust patient position: this may move cannula position relative to each other, and also affect venous return, and thus change amount of recirculation.
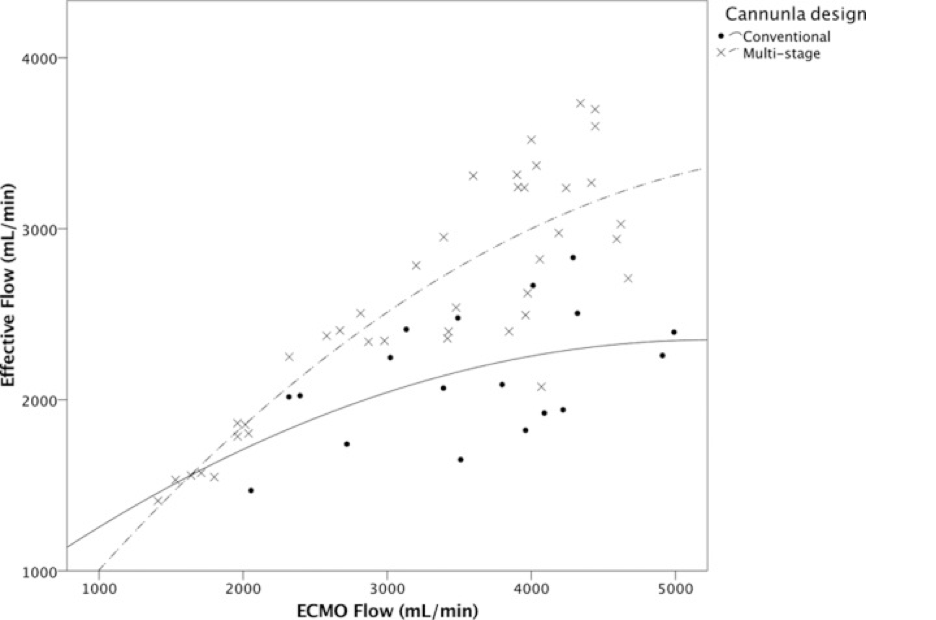
- Reduce ECMO flow (See Figure 3, below)
- Reposition ECMO cannulae (withdraw cannula or reconfigure circuit)
- Increase volume state, though this is rarely effective.
Learn more by reading the Alfred ICU guideline on Recirculation at ECMO.ICU
The jugular cannula was withdrawn 3cm and the saturations improved. However one week later the patient’s oxygenation deteriorated again and it is difficult to achieve Saturation > 88%. The D-dimer has increased to 30. A pre and post oxygenator gas are taken and show the following:
- PBO2 (Pre): 45 mmHg
- PBO2 (Post) 120 mmHg
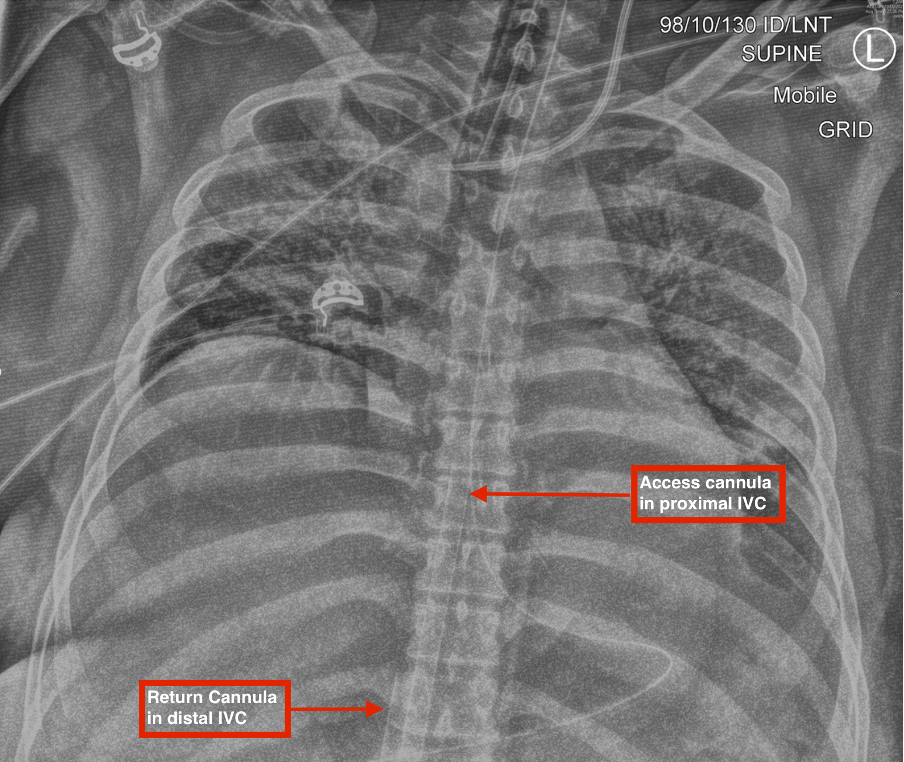
A repeat chest radiograph was obtained, see Figure 4 below.
Q4. What is the likely cause of the worsened oxygenation?
Oxygenator failure.
Over time fibrin deposition will reduce oxygenator efficiency and eventually may necessitate a circuit change (see Figure 5, below).
Post oxygenator oxygen tension (PBO2 (Post)) should normally be at least 200 mmHg. A lower value suggests oxygenator dysfunction and should prompt consideration of the need for a circuit change. A lack of colour differential may also be seen, with dark blood in both the access and return lines. Oxygen supply failure should also be excluded.
Note that the jugular return and femoral access cannulae appear to be well separated on the chest radiograph (see Figure 4), which together with the pre- and post-oxygenator gases, effectively excludes significant ongoing recirculation.

Learn more by reading the Alfred ICU guideline on Oxygenator failure at ECMO.ICU
References
- Conrad SA, Wang D. Evaluation of Recirculation During Venovenous Extracorporeal Membrane Oxygenation Using Computational Fluid Dynamics Incorporating Fluid-Structure Interaction. ASAIO J. 2021;67(8):943-953. doi:10.1097/MAT.0000000000001314 https://pubmed.ncbi.nlm.nih.gov/33315664/
- Palmér O, Palmér K, Hultman J, Broman M. Cannula Design and Recirculation During Venovenous Extracorporeal Membrane Oxygenation. ASAIO J. 2016;62(6):737-742. doi:10.1097/MAT.0000000000000440 https://pubmed.ncbi.nlm.nih.gov/27660904/
All case-based scenarios on INTENSIVE are fictional. They may include realistic non-identifiable clinical data and are derived from learning points taken from clinical practice. Clinical details are not those of any particular person; they are created to add educational value to the scenarios.