Everything ECMO 042: SIG alarm
Author: Dr Jeremy Smith, Dr Brooke Riley
Reviewer: A/Prof Chris Nickson
A 45-year-old man with severe COVID pneumonia is on veno-venous (VV) extracorporeal membrane oxygenation (ECMO) support for his respiratory failure. You are called to the bed space due to an ECMO alarm and note that the blood flow is no longer consistently displayed on the Rotaflow console screen.
Instead, you see this:
Q1. What alarm is this and what does it mean?
SIG alarm.
A SIG alarm signifies a loss of flow signal on the Rotaflow console. This is usually due to inadequate coupling gel/cream between the ultrasonic flow sensor and the pump head.
There will be a flashing “SIG!” in place of the blood flow reading, alternating with a number or with ‘—-’. Some consoles may not show “SIG!” or a number and simply show “—-” during a SIG alarm.
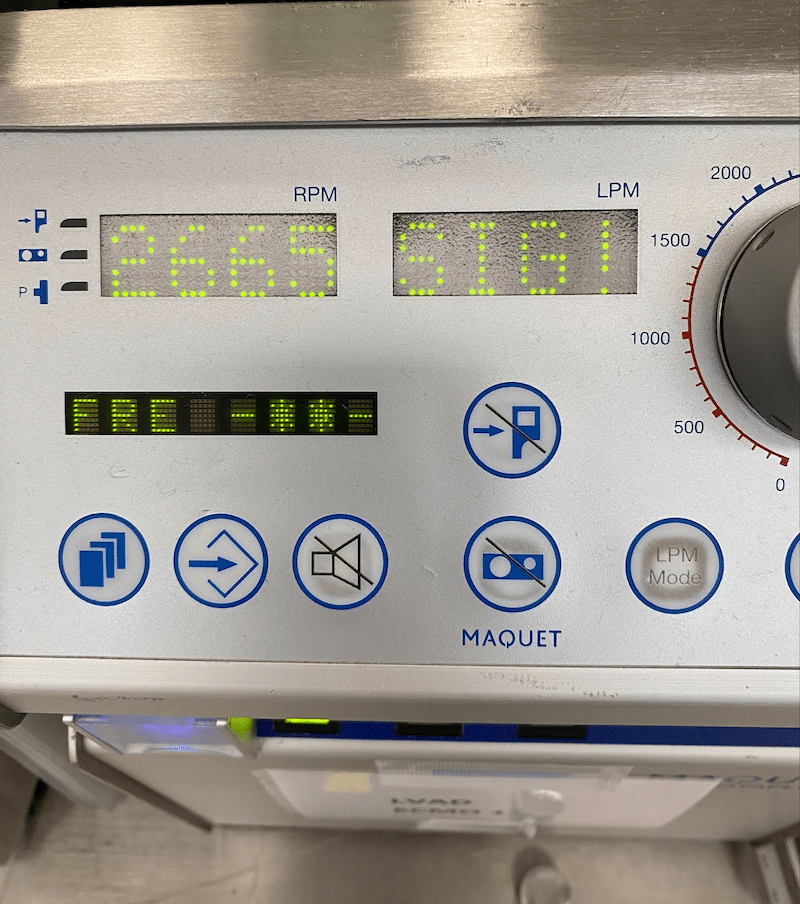
Figure 2. SIG alarm on Rotoflow console.
Q2. When might this alarm occur?
A SIG alarm can occur at any time, however more likely to occur the longer the circuit has been in use as the ultrasonic coupling gel/cream can disintegrate over time.
Q2. Which consoles can this alarm occur on?
This alarm only occurs on the Rotaflow (PLS) pump.
It cannot occur on the Cardiohelp (HLS) pump.
Q3. How does this alarm affect how the console runs?
In most circumstances it won’t affect how the console runs.
Blood will still pump through the ECMO circuit and the oxygenator will still work. However, the blood flow will not be displayed accurately.
Q4. What is important to check when this alarm occurs?
Priorities during a SIG alarm are:
- check the pump is still running (if not use emergency drive unit, aka hand-crank)
- check the patient is still supported by ECMO
Q5. How do we troubleshoot this alarm?
To obtain an accurate blood flow reading, and prevent the SIG alarm from occurring, the ultrasound coupling cream/gel needs to be replaced.
The steps to change this are as follows:
- Preoxygenate patient with 100% O2
- Talk through plan and ensure appropriate staff are available and aware of procedure (senior medical and nursing staff)
- Clamp circuit (post oxygenator)
- Decrease RPM to 0
- Open ultrasound cover and remove pump head
- Apply ultrasound coupling cream to ultrasound windows just distal to pump head
- Re-insert pump head, must be inserted with leading edge placed under pin and cover latched
- Increase RPM to 1500 and remove clamp
- Speed then increased gradually until desired flow is achieved
It is useful to have at least a 3 person team so that the procedure is performed rapidly and smoothly: one person on console, one to move pump head, and one to apply gel and clamp.
Q6. What are the potential issues during troubleshooting?
If the pump head is removed while still spinning an error occurs which requires the ECMO machine to be restarted. If this occurs the pump head should be placed in the emergency hand-crank until the ECMO machine is ready to use. The steps for part 6 would then need to be followed to change it back to the magnetic pump.
The other potential issues depend on the type of support the patient is on.
For VA:
- The patient may arrest during the change if they are completed supported. In this circumstance usually there is no requirement for CPR as the patient’s circulation will return on re-initiation of flow from the ECMO circuit.
For VV:
- Hypoxia is the main concern, which in severe circumstances can lead to bradycardic arrest which will require CPR if occurs. Often this is only required for a short period until oxygenation is returned via the ECMO circuit.
References
- Alfred ICU ECMO Guideline. SIG alarm [Accessed 18 Aug 2022]. Available at URL: https://ecmo.icu/emergency-alarms/?kw=sig+alarm#pageautoanchor-3
- Maquet. User’s Manual: Rotaflow with ICU Kit, Rotaflow System 1st ed. [Accessed 17 August 2022] Availabel at URL: https://www.manualslib.com/manual/2314593/Maquet-Rotaflow.html
