As prepared by Yannick Planche, here are the practice written questions from a recent CICM Second Part exam practice session at The Alfred ICU, with recommended reading from LITFL.com Critical Care Compendium and other FOAM sources:
Q1. a) Discuss the investigations relevant to the diagnosis and classification of pulmonary hypertension (PH) (7 marks)
Investigations
- PH defined as mean pulmonary artery pressure ³ 25mmHg
- Tests should focus on
- confirming diagnosis (echocardiography, RH catheterisation)
- classifying type PH (bloods, RFT, echocardiography)
- and grading severity (echocardiography, RH catheterisation)
- Bloods – BNP (?RHF), ANA/ENA (?CTD), ACE (?sarcoidosis), LFT (?PHTN), HIV serology
- ECG – ?RH strain or RVH (RAD, RBBB, dom R V1, dom S V5,6), ?large RA (p-pulmonale)
- Echocardiography – ?RH dysfunction, ?LH disease, ?valvular disease, ?PASP
- Respiratory Function Tests – ?COPD ?RLD ?normal spirometry low DLCO
- RH Catheterisation – confirm PH (mPASP > 25), ?PAH (PVR > 3 woods), ?RH Fx (CI)
Classification of Pulmonary Hypertension (PH)
- Pulmonary Arterial Hypertension (PAH)
- Idiopathic
- Heritable
- Drug/toxin induced (e.g. amphetamines)
- Associated (CTD, HIV, portal HTN)
- Responders to CCB
- Left Heart Disease
- HFrEF
- HFpEF
- Valvular disease
- Lung disease / chronic hypoxia
- Obstructive lung disease
- Restrictive lung disease
- Hypoxia (obesity-hypoventilation)
- Pulmonary artery obstructions
- Chronic thromboembolic PH (CTEPH)
- Other
- Multifactorial aetiology
- Hematological disorders (e.g. sickle cell)
- Systemic disorders (e.g. sarcoidosis)
- Complex congenital heart disease
- Other
1 b) Explain the biological pathways targeted in the treatment of pulmonary arterial hypertension (3 marks)
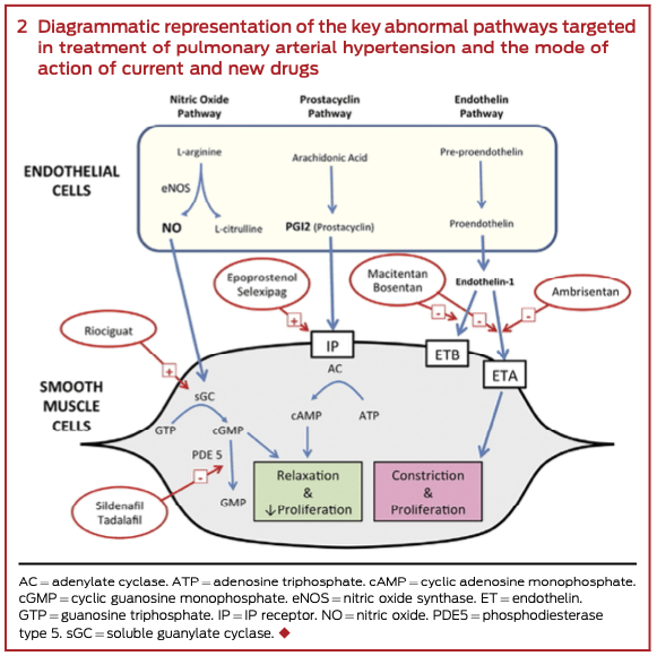
REFERENCES:
JAMA. 2022;327(14):1379-1391. https://doi.org/10.1001/jama.2022.4402
MJA 2016; 205(6): 271-276. https://doi.org/10.5694/mja16.00468
Q2. Discuss the assessment and management of a potentially lethal drug overdose (10 marks)
Assessment
- History
- Agent(s)
- Dose(s)
- Time since ingestion
- Clinical features and progress
- Patient factors (weight and co-morbidities)
- Investigations
- [drug] – blood and urine
- UEC – renal failure? hypoK+? hyperK+?
- ABG – acidosis? hyperBSL? hypercapnia? hypoxia?
- CK – rhabdomyolysis?
- osmolar gap – toxic alcohol?
- CXR – aspiration? NGT placement?
- ECG – rate, rhythm, PR, QRS, QTc, domR in AVR
Resuscitation
- Always secure ABC first
- Consult early with toxicologist
- Seek and treat complications of overdose
- Hyperthermia
- Hypoglycaemia
- Seizures
Decontamination
Activated Charcoal
- within 1hr ingestion
- 50g (adult); 1g/kg (kids)
- indications
- aspirin
- paracetamol
- digoxin
- TCA
- theophylline
- phenobarbitone
- paraquat
Multi-dose Activated Charcoal (MDAC)
- initial 50g bolus
- then 25g Q2H
- rarely useful > 6hrs
- indications
- massive paracetamol OD
- phenobarbitone coma
- carbamazebine coma
- theophylline OD
Enhanced Elimination
Urinary Alkalisation
- NaHCO3 iv 1-2mM/kg bolus
- then infusion 150mM over 4hrs
- frequent FWT; aim pH > 7.5
- regular K+ replacement
- monitor HCO3 and K+ Q4H
- continue until improving (clinical, lab)
- indicated drugs
- salicylates
- phenobarbitone
Haemodialysis (indications)
- toxic alcohols
- lithium (severe chronic)
- salicylate (severe)
- phenobarbitone (coma)
- carbamazepine (massive OD)
- valproate (massive OD)
- theophylline OD
- metformin (lactic acidosis)
- paraquat (charcoal haemoperfusion)
Antidote Therapy
- Commence as early as possible
- In consultation with toxicologist
- May be empirically indicated during CPR
- (e.g. NaHCO3, atropine, naloxone, digibind)
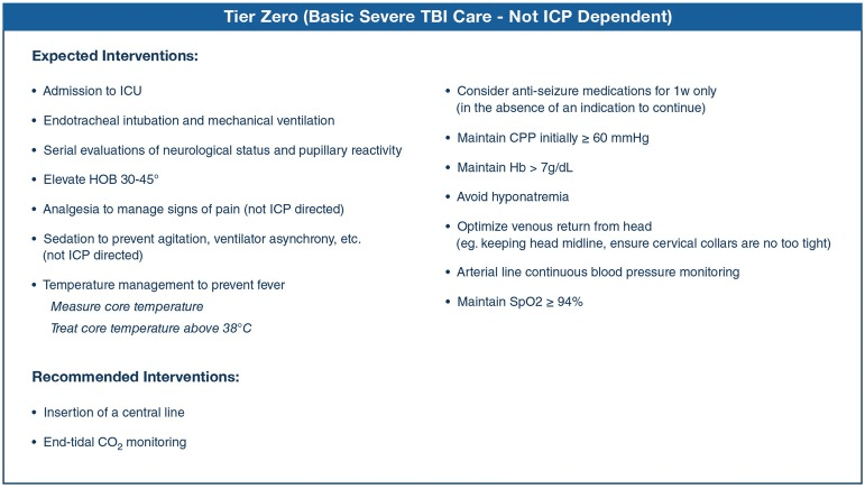
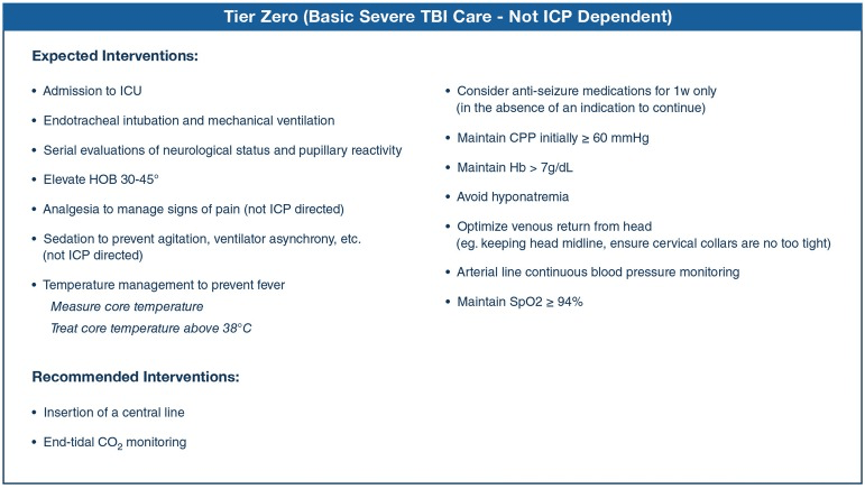
Q3. a) Discuss the basic management of any patient with a severe, acute traumatic brain injury (TBI) (4 marks)
3 b) Discuss the management of intracranial hypertension in patients with TBI (4 marks)
3 c) Discuss the role of hypothermia in the management of TBI. Cite any relevant evidence. (2 marks)
- Supposed benefit in the prevention of secondary neurological injury
- There is no role for the use of hypothermia in the routine management of TBI
- Two landmark trials
- EUROtherm3235
- cooling in patients with sustained ICH in the setting of TBI
- increased mortality in cooling group
- and increased incidence of poor neurological outcomes
- POLAR 2018
- therapeutic cooling of patients with severe TBI due to blunt trauma
- no benefit in neurological outcomes or mortality
- increased risk of infection and prolonged MV duration
REFERENCES:
Intensive Care Med. 2019; 45(12): 1783–1794. https://doi.org/10.1007%2Fs00134-019-05805-9
JAMA 2018 Dec 4;320(21):2211-2220. https://doi.org/10.1001/jama.2018.17075N Engl J Med 2015; 373:2403-2412 https://doi.org/10.1056/NEJMoa1507581
You can access all the previous practice questions since 2014 here:
https://docs.google.com/document/d/1_Ta8IvVaVtc5Il7-kJwj6qKGu54OmifJGRUWCXud8dY/
See this link on INTENSIVE for exam resources: https://intensiveblog.com/resources/#3