Labs and Lytes 009
Author: Anonymous
Reviewer: Chris Nickson
A 40 year-old man fell from a multi-story building. He sustained multiple traumatic injuries including a severe head injury. After 10 days in ICU he became increasingly tachypneic with a respiratory alkalosis, then was noted to have rhythmic right arm and facial jerking and developed a fixed, dilated right pupil. He was given treatment to lower his intra-cranial pressure, including hypertonic saline and a thiopentone infusion.
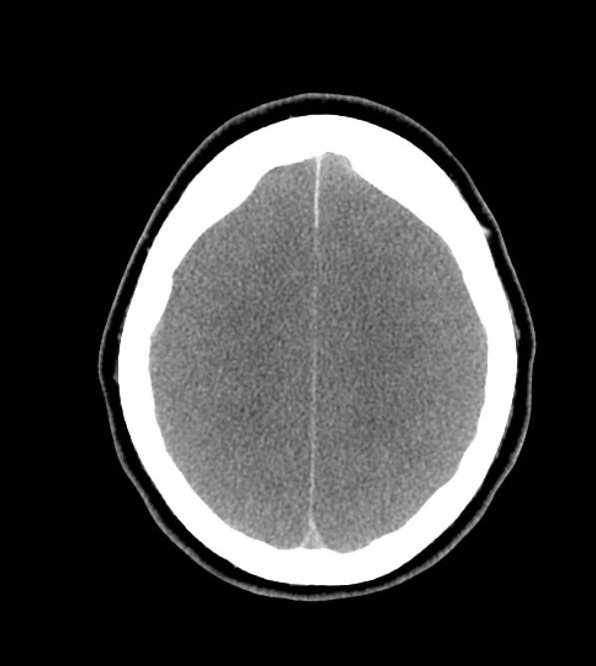
An urgent non-contrast CT head was performed; two axial slices are shown below:
Q1. What are the CT head findings?
- Diffuse cerebral oedema, with loss of grey-white matter differentiation
- Complete effacement of sulcal spaces, and partial effacement of the ventricles
- Relative hyperdensity of the basal cisterns and sulci, HU 35-40, in keeping with pseudo subarachnoid haemorrhage
- Uncal herniation effacing the basal cisterns
Q2. What is pseudo-subarachnoid haemorrhage?
This is a CT head finding seen in patients with severe cerebral oedema characterised by relative hyperdensity of the basal cisterns and sulci
Theoretically due to:
- Displacement of low attenuated CSF by increased pressure
- Distension of the superficial vasculature
- Oedema of the adjacent cortex
Following the CT head the patient was reassessed and his progress was discussed with his family. A procedure was then performed.
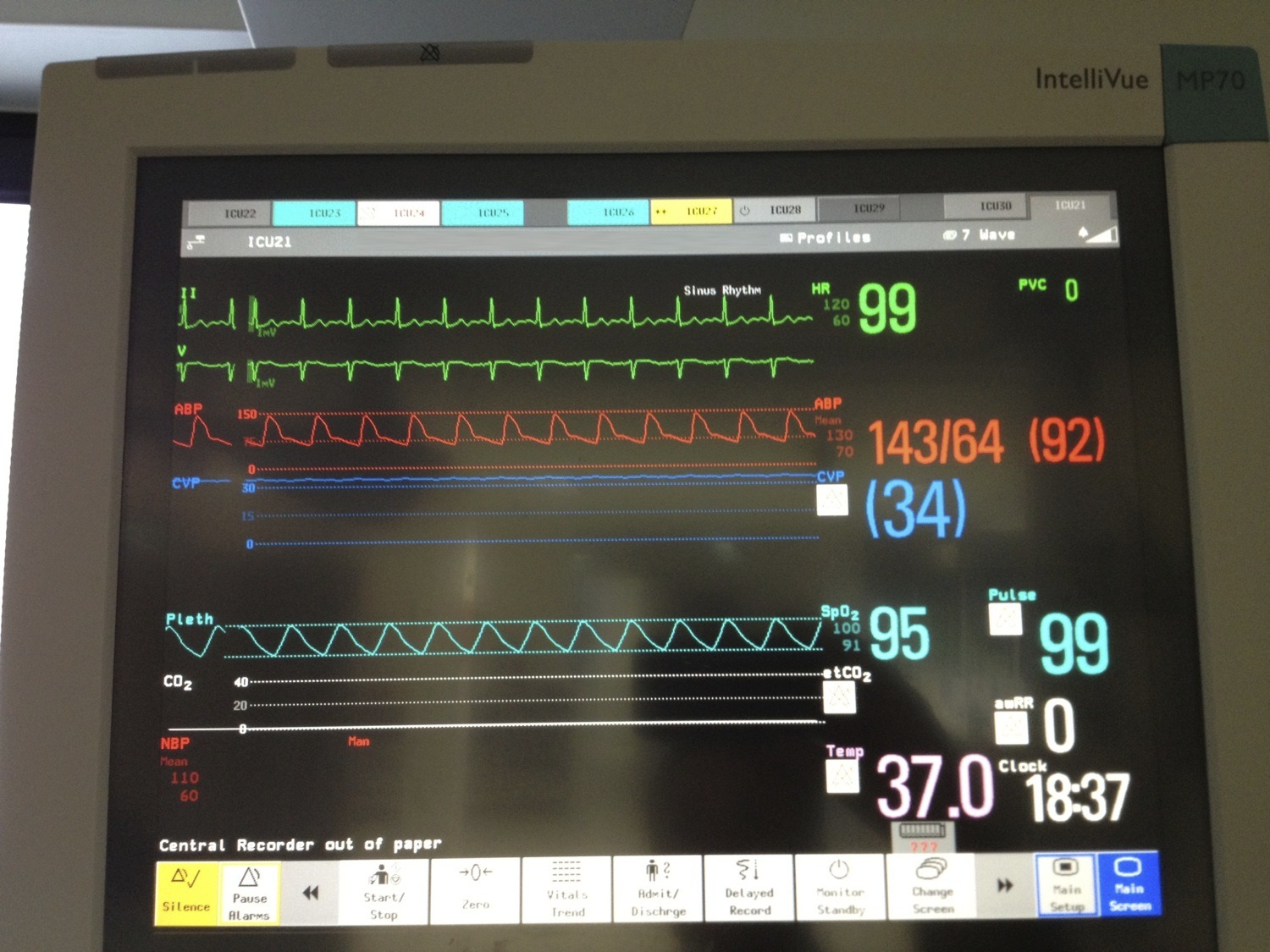
During the procedure the patient’s monitor showed the following:
Q3. What procedure is being performed?
An apnoea test as part of clinical brain death testing, as indicated by the continuous ETCO2 reading of zero
Brain death testing involves demonstration of:
- absence of responsiveness
- absence of brainstem reflexes
- apnoea
There is also an incidental finding of elevated CVP with a flat trace, which may be artifactual.
Q4. What are the preconditions for this procedure?
Preconditions:
- cause for coma consistent with brain death
- at least 4 hours of observation during which other preconditions must be met (GCS 3, pupil non-reactive, no cough, apnoea)
- neuro-imaging consistent with acute brain pathology that could cause brain death
- normothermia (T>35C)
- normotension (SBP>90 or MAP>60mmHg in an adult)
- no sedation or analgesia (dependent on types of drugs used, renal and hepatic function; use antagonists if concerned)
- absence of severe electrolyte, metabolic and endocrine disturbances (glucose, Na+, PO43-, Mg2+, renal and hepatic function)
- no paralysis (use NMJ monitor or electromyography if concerned)
- ability to assess brain stem reflexes (at least one eye and ear)
- ability to perform apnoea test (doesn’t have severe hypoxic respiratory failure or have a high cervical spine injury)
Q5. How is the procedure performed?
Apnoea testing procedure
- Hyper-oxygenate for a period of 10min with 100% FiO2
- Ventilator is weaned (PEEP to 5, eucapnoea)
- Baseline ABG is taken
- If pt stable and SaO2>95% then patient can be disconnected from ventilator
- Oxygen is administered via a tracheal cannula (2L/min) or via CPAP (10cm H2O)
- Visual observation: 8-10min duration
- Repeat ABG prior to reconnection to the ventilator (expect rise of ~3 mmHg/min in PCO2 unless high O2 flow)
The test is deemed positive (consistent with brain death) if:
No respiratory response to:
- PaCO2 > 60mmHg (or an increase of 20mmHg)
- final arterial pH <7.3
References
- ANZICS Statement on Death and Organ Donation – 3.1 (2010)
- Radiopaedia.org — Diffuse axonal injury
- Radiopaedia.org — Pseudo-subarachnoid haemorrhage
- LITFL CCC — Brain Death
All case-based scenarios on INTENSIVE are fictional. They may include realistic non-identifiable clinical data and are derived from learning points taken from clinical practice. Clinical details are not those of any particular person; they are created to add educational value to the scenarios.