Q1
Discuss the physiology of the foetal circulation and its transition to the neonatal circulation
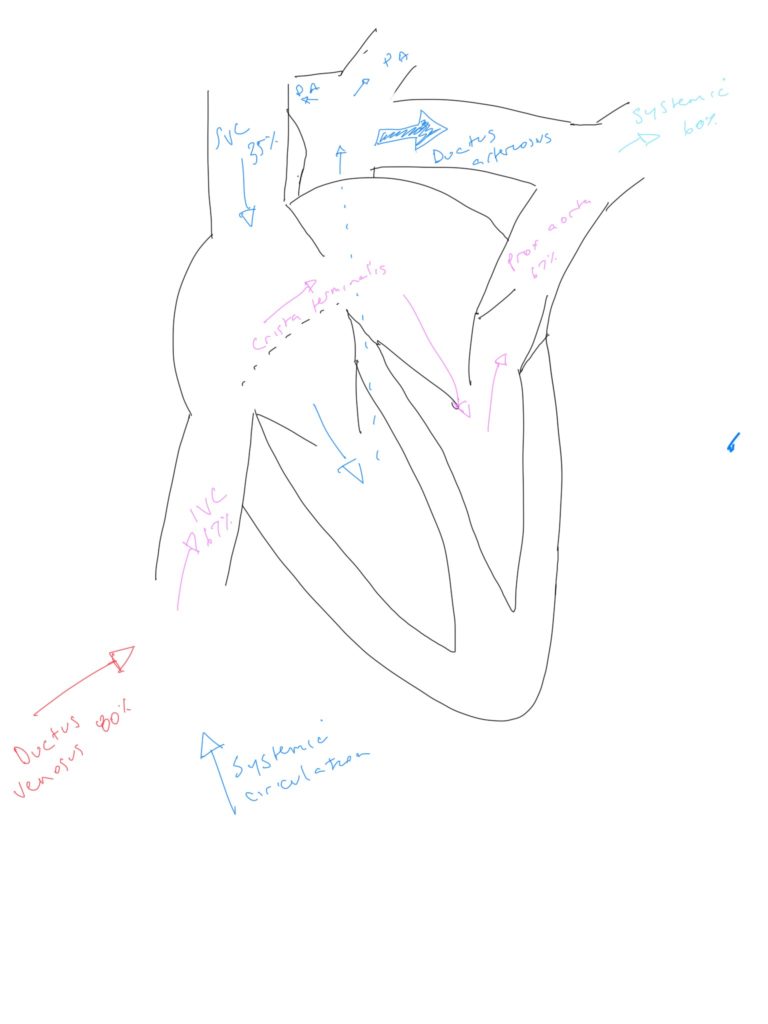
Foetal circulation:
- The foetal circulation derives its oxygenation, nutrients, waste removal from the placenta
- Blood flow to the placenta is via the umbilical artery (240mL/min at term), branches of the internal iliac arteries
- It is oxygenated to an SaO2 of 80% (30mmHg), then returns via the umbilical vein
- The umbilical vein reenters the foetus via the cord, then the left branch of the hepatic portal vein
- 60% of this blood bypasses the liver to the IVC in the ductus venosus
- This blood enters the RA, and 60% of it is directed by the crista terminalis across the formaen ovale to the LA – this results in more richly oxygenated blood entering LV
- LV and RV work in parallel via a series of shunts
- LV and RV are of equal thickness
- Pulmonary vascular resistance is high (due to collapse of the lungs), thus receiving only 10% of RV output
- Most of the RV output is shunted via the foramen ovale (a communication between right and left atria) and ductus arteriosus (communication between PA and aorta) to the systemic circulation:
- Venous return to the RA comes from two sources – the SVC and the IVC
- The IVC blood is more richly oxygenated, and is directed preferentially into the LA (hence LV) via the foramen ovale
- The SVC blood has a lower O2 content (returning from the brain) at 40%
- This blood is directed largely into the PA. Most of it (90%) is diverted across the ductus arteriosus into the descending aorta
- Thus the coronaries/brain receive more highly oxygenated blood than the structures distal to the arch of the aorta
- Both foetal and neonatal circulations are heart rate dependant due to a relatively fixed stroke volume, so bradycardia will be poorly tolerated.
- Normal range 120-160 bpm
- During contractions foetal tachyardia may occur due to cranial compression.
- Early decelerations can also occur due to cranial compressions and rising vagal tone.
- Late decels are due to hypoxia.
Transitional circulation
- At birth, the neonatal circulation must transition from a parallel to series circulation
- There are 3 key events:
- Loss of low resistance placental circuit
- Precipitous fall in PVR with first breath
- Closure of ductus arteriosus and reducation/cessation of foramen ovale flow
- When the umbilical cord is clamped/constricts at birth this low resistance circuit is lost
- SVR rises
- After the first breath the lungs expand and become oxygenated
- These changes cause a drop in PVR and an increase in pulmonary blood flow
- Left atrial pressure rises with increased venous return
- Right atrial pressure falls
- The foramen ovale closes, and in most patients fuses over the subsequent 4-6 weeks
- The ductus arteriosus contains spiral smooth muscle
- This contracts due to increased PaO2, decreased circulating PGE1 and PGE2 over 10-15 hours. This thromboses over the subsequent 2-3 weeks
- The ductus venosus closes a few hours after birth, triggering factors are unclear
- LV wall thickness increases by about 50% at 6 months