Author: Ruth O’Leary
Peer reviewers: Arne Diehl, Paul Nixon, Jayne Sheldrake
Everything ECMO 024
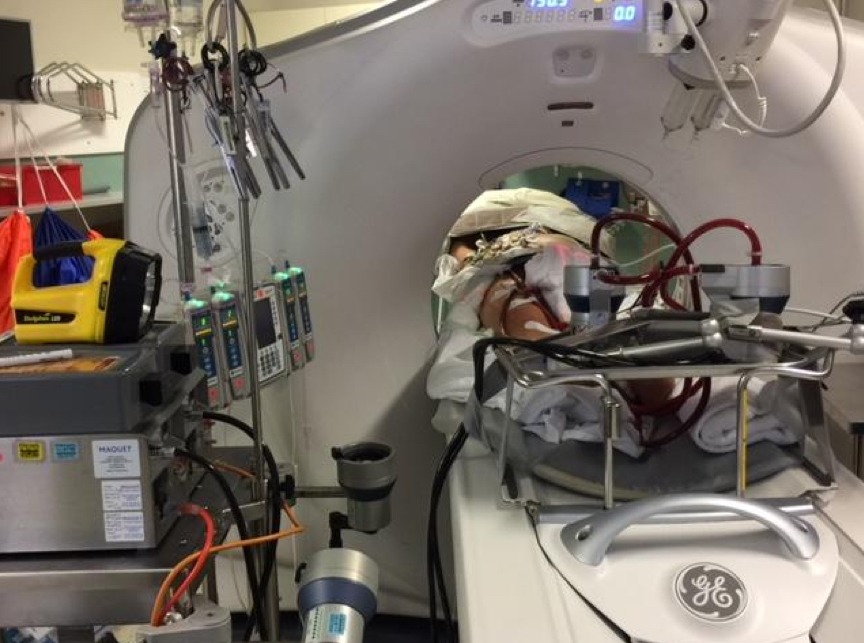
A 52-year-old male is admitted to the intensive care unit with decompensated dilated cardiomyopathy and cardiogenic shock. He fails to improve with optimal inotropic support and is commenced on V-A ECMO. After 72 hours on ECMO sedation is ceased to assess neurology. The patient fails to wake appropriately and due to lateralising neurological signs, a CT Brain is deemed necessary.
Q1. What are the specific issues with transporting this patient to CT?
Intrahospital transport of critically ill patients is a potentially dangerous procedure, with a significant risk of adverse incidents. Transfer of ECMO patients adds a layer of complexity, requiring personnel who are competent in troubleshooting problems with the circuit. Thus this patient requires sufficient personnel to manage the ECMO circuit and also attend to the patient and all their other equipment, including ventilator and infusions. In view of these complexities, it is important to weigh up the risks and benefits of performing the scan and ideally to perform the transfer during daytime hours when staffing is optimal. In addition to the general concerns discussed, it is important to be aware of the battery life of the ECMO console (discussed below).
Q2. You are informed that the main CT scanner is broken and the only available scanner is located approximately eight minutes walk away. How long is the battery life of an ECLS console?
The battery life of an ECMO console depends on the age of the battery, the speed of the pump (rpm) and the return pressure in the circuit. The patient’s mean arterial pressure, the resistance in the return limb and the size of the return cannula all contribute to this return pressure. At higher speeds, the battery life is reduced. New HLS (Cardiohelp) and PLS (Rotaflow) consoles have sufficient battery for 90mins at 3000rpm producing 5L/min flow. As with other electronic devices, this reduces as the battery ages.
The PLS console battery life is displayed in a Voltage format. It is fully charged at 27.4V. Assessment of the battery status should occur 2-3min after disconnection from power. It may drop a couple of volts but should then stabilise and remain above 24V before starting the transfer. When disconnected from a power source there is an alarm to indicate that the pump is on battery. Once this alarm is silenced there is no further alarm until the battery reaches 20V. Once the battery falls to 20V there is a continuous alarm that is unable to be silenced. The pump will stop at 19V.
The HLS console battery life is displayed in actual time remaining (e.g. 45mins) as well as percentage battery charged. We monitor the battery using percentage charged. When disconnected from a power source there is an alarm to indicate that the pump is on battery. Once the percentage charged falls to 20% the alarm LED flashes once per second. The alarm LED flashes twice per second when the battery charge falls below 10%.
Q3. What equipment is necessary during transport?
When planning the transport of an ECMO patient consider both specific ECMO equipment and general equipment for transporting an ICU patient. All patient transfers should include airway equipment and adequate infusions including sedation, anticoagulation and inopressors. Extension lines should be added to all infusions to ensure adequate length. Consideration should be given to the ventilator, as these patients may not be sufficiently stable for a transport ventilator. Two oxygen tanks are required – one tank for the ventilator and a separate tank for the ECMO oxygenator. For all ECMO transfers, you must bring ECMO safety equipment – clamps for circuit breach or failure, a hand crank in an accessible position and a trolley (or bed bridge) for transport of the console.
Q4. How many personnel are required for the transfer?
In order to safely transfer an ECMO patient at a bare minimum, you need two ECMO accredited staff (e.g. one ECMO accredited ICU nurse or perfusionist and one ECMO accredited SR or consultant). In addition, you need sufficient personnel to move the ventilator, infusions, ECMO and patient as well as personnel who are appropriately experienced to deal with any adverse incidents that arise. On average you are likely to need 5 staff members – one for airway and ventilator, one for infusion pumps, one to move the bed, one to move the console and one to mind the ECMO cannulae.
Q5. What complications should be anticipated during the transport?
As with all transports of critically ill patients, it is important to discuss contingency plans prior to embarking on a transport. In addition to adverse incidents that may occur with any ICU transfer you should consider:
- Battery failure – note the position of the hand crank
- Cannula displacement – confirm the presence of adequate clamps
- Circuit rupture – ensure that the cannulae are minded at all times to avoid damage
- Flow issues or access insufficiency due to inadequate sedation or paralysis, or patient position especially when moving onto the CT scanner
- Hypothermia – the heater/cooler device does not run on battery, which can lead to rapid drops in core temperature, particularly at higher flow rates.
Q6. What actions should be taken in the event of an ECMO related complication?
Actions required depend on the type of ECMO complication:
- Battery failure – switch circuit to hand crank and maintain same rpm as patient was on previously
- Cannula displacement
- Partial – secure cannula and reassess immediately when returned to the unit
- Complete – clamp circuit and compress site. Support patient using conventional support and call for help
- Circuit rupture – clamp the circuit and call for help.
- Hypothermia – connect the heater/cooler as soon as possible. Take preventive measures if longer transfer or cold environment anticipated.
Q7. You need to fit in a lift – how are you going to get all the equipment in there?
Transporting ECMO patients by lift can be challenging due to the number of personnel required and the volume of equipment. It is important to ensure that the largest lift is used – many hospitals have different sized lifts for patient or visitor access. Moving in and out of the lift is a high-risk time, so ensure that adequate time and care is taken to optimally load the lift. Consider sending certain personnel via a second lift or stairs to minimize the load (As with all transports, ensure all vital equipment and staff enter the lift with the patient).
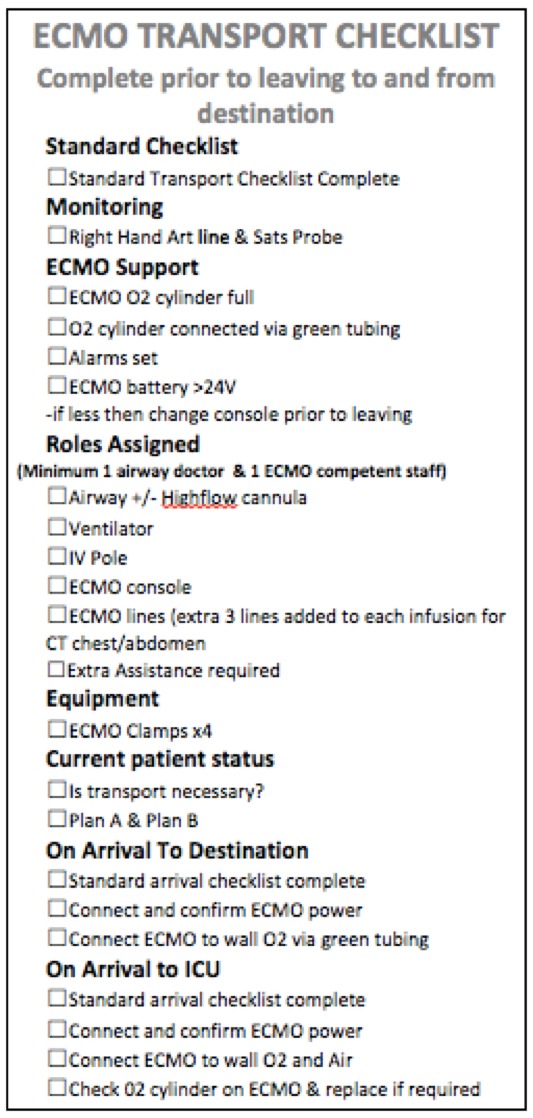
Q8. Are any special procedures required on arrival at the CT scanner?
On arrival to CT the patient should be reassessed. In addition to standard transport procedure (e.g. plugging in ventilator and pumps; attaching ventilator to wall O2) the ECMO console should be plugged in and AC power should be confirmed. The ECMO oxygenator should then be connected to wall oxygen via the green tubing at the same rate as previously. Given the complexity of ECMO transfers an additional ECMO checklist is useful as a prompt. An example from the Alfred Hospital is included below.