Labs and Lytes 027
Author: Eamon Raith
Reviewers: Sarah Yong, Chris Nickson
A 25-year-old man was admitted to ICU post PEA arrest from haemorrhagic shock, following an assault and penetrating injuries to his right thigh and scrotum. In ICU he develops ischaemic hepatitis secondary to hypoxia, coagulopathy and acute kidney injury. He requires inotropic support, CVVHDF and repeat blood product transfusions.
Two weeks later the patient deteriorates and requires re-siting of his lines. A left internal jugular CVC and left subclavian VasCath are inserted with ease, under dynamic ultrasound guidance.
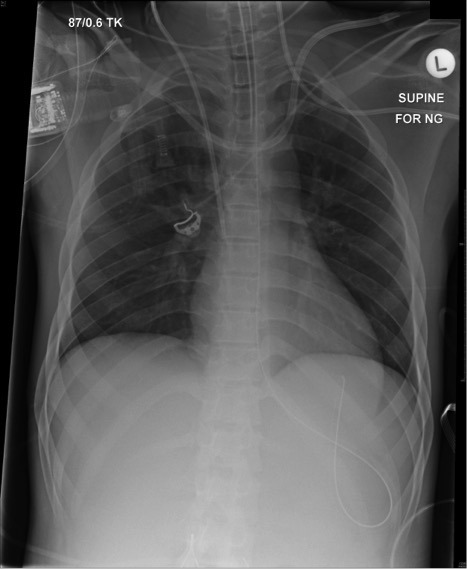
An X-ray is obtained prior to removal of the existing right IJV CVC:
Q1. Describe and interpret the chest radiograph (CXR)
This is a supine AP CXR.
The most striking findings are that of inappropriately sited vascular catheters:
- Left subclavian CVC, which has tracked up the left internal jugular vein (tip not visible)
- Left internal jugular vascath, which has traversed the midline to enter the right brachiocephalic vein, with the tip within the right subclavian vein
Other findings:
- Hardware: ETT, nasogastric tube, Right internal jugular CVC all appropriately placed
- No lung parenchymal or cardio-mediastinal pathology, no fractures or lytic lesions, normal soft tissues
Q2. Outline the indications for a CVC.
Indications for CVC insertion include1:
- Intravenous access (especially if difficult peripheral access)
- CVP monitoring
- ScVO2 monitoring / sampling
- Administration of irritant substances (eg vasoactives, TPN, chemotherapy)
- Renal replacement therapy, plasmapharesis, apharesis
- Cardiac catheterization
- Transvenous cardiac pacing
Q3. What is the ideal catheter tip placement?
Ideal catheter tip placement is widely accepted as being1;
- In the largest central vein possible (typically SVC or IVC)
- Ideally outside the pericardial sac
- Parallel with the long axis of the vein, so as to prevent the catheter abutting the vein or heart wall at an acute angle or end-on
Q4. Define ‘catheter misplacement’, and explain the different types of misplacement.
Misplacement of a CVC refers to any catheter whose tip does not lie in an ideal position. It can occur at the time of insertion or the tip can migrate over time.1
The site and frequency of catheter misplacement varies with the site of insertion, the insertion technique, and patient positioning.1 Catheter misplacement may be intravenous, arterial or extravascular.
Intravenous misplacement:
- Relatively common when x-ray screening is not used
- More frequent with subclavian or left-sided approaches due to the presence of corners
- A malpositioned IV catheter should be repositioned, replaced or removed as soon as possible.
Arterial puncture:
- A common complication, particularly at the right IJ and both femoral vein insertion sites
- ncidence is 1-11%.1
- Arterial cannulation is usually obvious, from the colour and pulsatile nature of backflow
- Once cannulated, removal of large-bore catheters from arteries may risk distal ischaemia from haematoma, dislodged emboli and lack of blood flow
- Surgical removal may be necessitated.
Extravascular misplacement:
- May occur at insertion (guidewire insertion, dilation) or later (tip migration)
- the risk associated with early haemorrhage is bleeding into low-pressure spaces (e.g. pericardium).
- Perforation into the pericardium may occur due to erosion by the catheter tip resulting in RA or lower SVC perforation.1
- Once clinical suspicion is raised, the diagnosis can be confirmed on echocardiography, and aspiration of infused fluid should be attempted through the catheter, and urgent pericardiocentesis, stenting or surgical repair performed.
Catheters may similarly migrate to the pleural space, the mediastinum or other sites.
Catheter tip migration after insertion is dependent on;
- Phase of respiration
- Catheter type
- Insertion site
- Body habitus
- Development of a clot
- Body position.1
Q5. How should misplaced CVCs be managed?
Management depends on the location of the catheter, indication for central access, and the clinical condition of the patient. If there is suspicion that a catheter may be misplaced, then risks associated with removal must be considered, particularly that of uncontrolled haemorrhage – i.e. “If in doubt don’t take it out.1 Assessment of the misplaced catheter should include consideration of the following1: If the answer to all of these questions is yes, the catheter is in a central vein and can be used. This table, from Gibson and Bodenham, can be used as a guide to the identification of misplaced catheters.1
Q6. Describe the CVP waveform
References and Links
- Gibson F, Bodenham A. Misplaced central venous catheters: applied anatomy and practical management. British journal of anaesthesia. 110(3):333-46. 2013. [pubmed] [free full text]
- Interpretation fo the central venous pressure waveform (Deranged Physiology). URL: http://www.derangedphysiology.com/main/core-topics-intensive-care/haemodynamic-monitoring/Chapter%202.1.3/interpretation-central-venous-pressure-waveform