Author: Aidan Burrell
Reviewers: Josh Ihle, Chris Nickson
Everything ECMO 010
A 45-year-old lady with ARDS remains hypoxic despite mechanical ventilation, proning, and nitric oxide. She has a central venous catheter (CVC) in the left femoral vein, and an arterial line in the right femoral artery.
You prepare her for VV ECMO cannulation.
Q1. Describe the equipment you require to perform VV ECMO cannulation.
ECMO cannulas are long, wide, wire reinforced cannulas. The venous cannulas (figure 1) can be single-stage or multi-stage. Single stage cannulas only have holes at the distal tip (figure 1, bottom cannula) whereas multi-stage cannulas have multiple access points along the cannula that are designed to reduce suck down (figure 1, top cannula). They come in a variety of diameters and 19-27 Fr gauges are typically used. Lengths also vary and are chosen to accommodate different configurations – shorter cannula for the neck (15-25cms) and longer cannula (55cm) for the femoral vessels.

Figure 1. Distal tips of venous ECMO cannulas. Single-stage (bottom) and multi-stage (top).
Arterial cannulas (figure 2) are shorter, narrower (typically 15-23Fr), and often have a luer lock to connect to the distal perfusion cannula during VA ECMO. The arterial cannula can be also used in VV ECMO for the internal jugular vein. If this is chosen, the luer lock must be carefully closed. This prevents air embolism if used as an access cannula and prevents bleeding if used as a return cannula.
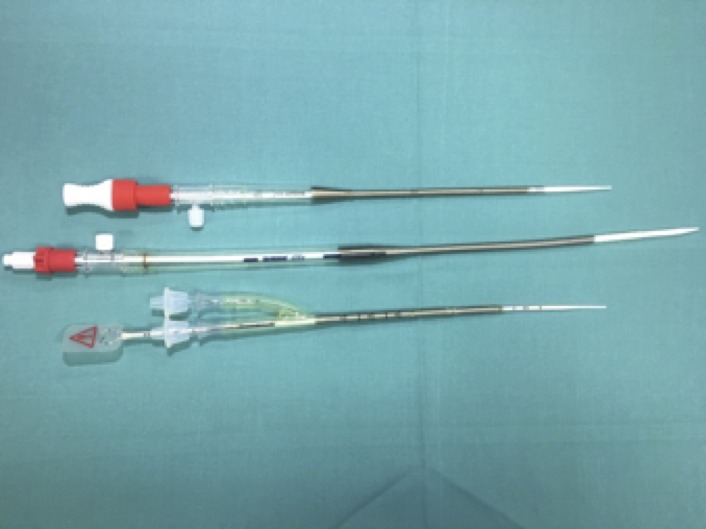
Figure 2. Arterial ECMO cannulas (top two with red caps)
Dilators come in a range of brands, such as Biomedicus, Cook and Avalon (figure 3). Different dilators have different characteristics.
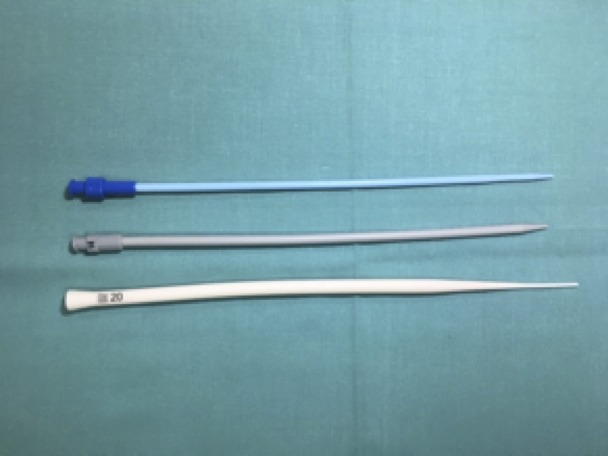
Figure 3. Dilators for ECMO cannulation (Biomedicus, Cook, and Avalon, from top to bottom)
Wires are very long (1.8m or 2.4m) and have J looped tips. There are soft wires and stiffer wires. The soft wires are safer in terms of minimising vascular injury, however, they are more easily bent by poor cannulation technique (figure 4). The stiff wires (i.e. Amplatz, figure 5) can make dilation much easier but come with a higher risk of inadvertent vascular injury despite having a flexible tip.

Figure 4. Soft wire (in right hand)
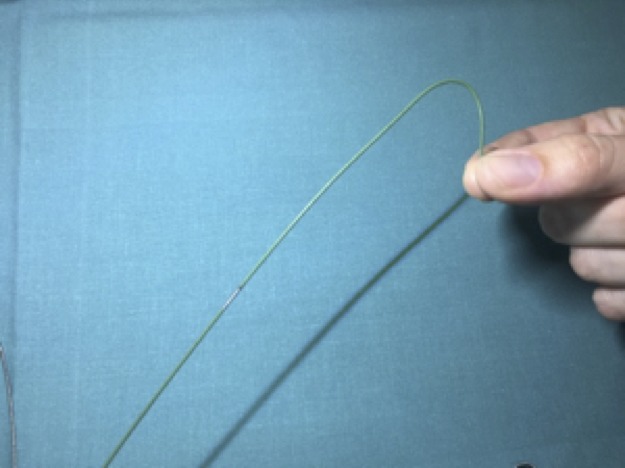
Figure 5. Amplatz stiff wire.
Q2. Where will you place the cannulas for VV ECMO? What are the advantages and disadvantages of the commonest two configurations?
At the Alfred ICU, a femoral-femoral configuration is usually preferred initially.
| Advantages | Disadvantages | |
| Femoral – femoral | Rapid access
Easier to place and secure Easier to transport |
Potentially less flow |
| Femoral – internal jugular vein (IJV) | Potentially higher flow | More recirculation
Securing IJV line is more complex |
Q3. Should you re-wire the existing lines?
No (in an ideal world!)
The risk of infection by re-wiring a cannula is high. The venous CVC should be removed and a new clean puncture performed. A new radial arterial line should be placed and the femoral arterial line also removed (arterial line placement can often be delayed until after the ECMO cannulation is completed).
ECMO cannulas have high rates of infection as they are large and often remain in situ for weeks. Thus insertion of new, clean lines using sterile technique is preferred. If an ECMO cannula does become infected it may be difficult to resite them depending on the access points available. Finally, ECMO cannulation requires a nice clean entry point into the vessel – an existing line may enter the vessel via a tortuous route. This may have been OK with a CVC, but will tend to cause problems with the stiffer ECMO dilators and cannulas. There have even been cases of CVCs that have transected an artery during insertion – this can be a catastrophic discovery to make when attempting a ‘rewiring’ for ECMO cannula insertion…
Q4. Your colleague says he has done many CVCs and can cannulate just fine using the landmark technique. What is the role of Ultrasound (US) during cannulation?
Ultrasound is essential for percutaneous cannulation.
Ultrasound:
- Increases first pass success
- Helps with vessel selection (e.g. left versus right)
- Identifies potential problems with the site (e.g DVT, calcification)
- Enables sizing of cannulas
- Enables confirmation of wire in the vein or artery
- Enables insertion in the correct part of a vessel (e.g. avoid bifurcation of the common femoral artery into superficial femoral artery and profunda)
- Identifies complications (thrombus, haematoma, pseudo aneurysm)
There is no role for a blind multiple passes technique of cannulation. This leads to delays, haematoma (so-called “porcupine injuries”), and later places the patient at higher risk of infection.
The bleeding risk from multiple failed passes increases once the patient is established on ECMO, and therapeutic heparinisation is commenced. Therefore, ensuring the femoral vessel is punctured on the first attempt, below the inguinal ligament is important. A retroperitoneal haemorrhage can be difficult to diagnosis and often presents very late – the use of ultrasound is important to minimise this risk!
Q5. Describe the key steps that you will take to place the needle into the vessel using the US?
It is important to maximise your first pass success rate to prevent hematoma or vasospasm formation
- Under full sterile conditions, identify a straight part of vessel
- Find the most superficial part of the vessel (without moving too high or low relative to other anatomical structures, e.g. the inguinal ligament, or vessel bifurcation)
- Aim for a flat entry into the vessel where possible (angle approx. 25-30 degrees)
- Avoid thrombosed or calcified vessels
- Enter the middle of vessel to ensure a clean entry
- Once in the vessel, advance the needle within the lumen a few more millimetres under vision to ensure the tip is well within lumen and wire will pass freely – maintain an acute (“flat”) angle to the vessel minimises the risk of inadvertent puncture of the posterior wall (“back-walling”).
- Hold the needle steady as you remove the syringe to prevent inadvertent removal of the needle. This is best done with an ‘underhand’ grip on the needle so that your hand rests on the patient and allows you to continuously visualise the needle entry point at the skin.
- Feed the wire. Do not advance if there is resistance — stop! When using an Amplatz stiff wire, be very careful as the distal end as it approaches the heart to avoid a penetrating injury.
- Confirm the wire course at the femoral vessel by visualising with ultrasound near the point of entry.
- Ideally have another ultrasonographer available to confirm the distal end of the wire is advanced to the IVC-RA junction when inserting a venous return cannula at the femoral site.
Q6. You bend the wire on insertion (doh!) – how does this occur and how can you prevent this from happening?
The wire is most commonly bent or ‘kinked’ during dilation, especially when using soft wires and larger French stiff dilators.
Kinking occurs when the dilators are advanced ‘off axis’ in a direction that does not follow the path of the wire (figure 6 – the dotted lines represent the direction of force during dilation). The dilator then moves past the point the wire enters the vessel and kinks the wire. In figure 7, the dilator was advanced in the incorrect direction, at a different angle to the original needle cannulation, and then the wire became twisted like a corkscrew during the sequential dilation and rotation process.
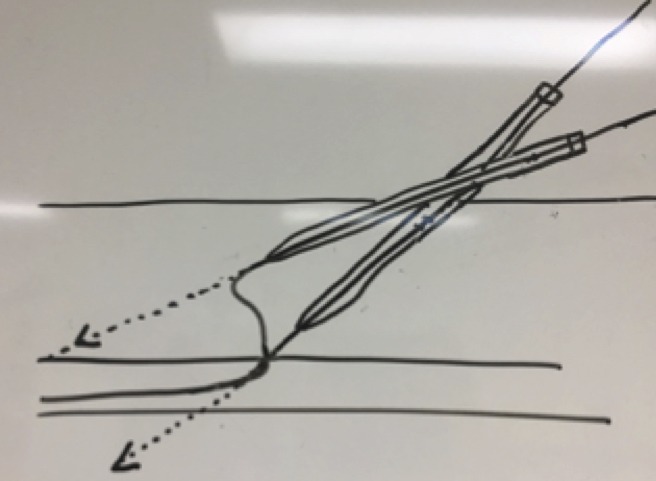
Figure 6. Mechanism of wire kinking during dilatation
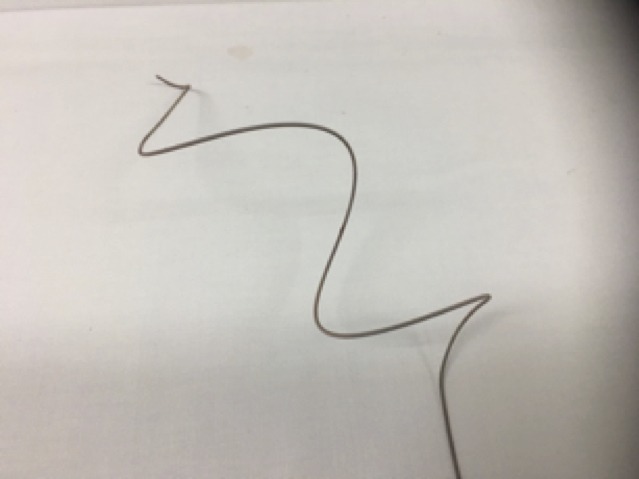
Figure 7. Yikes!
To help prevent this, the cannulator should be conscious of the trajectory of the needle and wire during insertion. Ensure dilators are advanced along the same path during subsequent dilatation.
Q7. The left femoral vein is 12mm. The right is 9mm. What size cannulas will you use?
The cannula size that fits inside a vessel can be estimated using this formula:
Vessel mm x3 = French gauge of cannula
In practice, other factors come into play as well:
- Size of the patient
- VA vs VV ECMO
— in general, VA ECMO requires lower blood flows, while sick VV ECMO patients with high cardiac outputs often require very high ECMO blood flows and bigger cannulas - Site of cannulation
- Access vs return
— As most problems occur on the access side, such as access insufficiency, a large cannula is important, although a small return cannula diameter will also increase resistance on the circuit and reduce ECMO blood flow.
As a general rule of thumb, try to use as large cannulas as possible that can be safely and quickly inserted. In this patient, a 25Fr multistage access cannula and a 19 Fr return cannula were used.
Q8. Describe the dilation technique you will perform to insert the cannulas?
Dilation can be done with one or two person techniques, and is influenced by time and staff availability, and whether or not you are using stiff wires.
The key principle is to sequentially dilate up the skin and tissues without causing tissue trauma. It is important to push the dilator along the direction of the wire (see question 6). Push the dilator in straight until there is resistance and then twist in one direction whilst maintaining forward pressure and torque, which will apply tension on the subcutaneous connective tissue fibres. When you withdraw the dilator, this loosens or tears the underlying connective tissue fibres making the next pass a little easier. Repeat the process, each time advancing the dilator further before twisting. Several ‘advance and twist’ attempts may be required with each dilator, be patient!
“It is like medical school, you go in straight and come out twisted!”
— Vin Pellegrino on sequential dilation for ECMO cannulation
If using a two person technique, the second person can jiggle (or “rack”) the wire in and out of the dilator to feel for “play” (free movement) and “hold up” (resistance to free movement). “Hold up” is the earliest signal that the wire is being bent or kinked when the dilator is moving NOT in line with the wire. If the second person feels any increase in resistance when jiggling the wire the cannulator must stop dilating and adjust the angle of dilator until the wire freely passes through the dilator again.
Q9. You are having difficulty passing the cannulas through the right skin. Do you cut the skin?
No (in an ideal world!)
This varies between centres – some do not cut the skin at all, while others routinely perform open incisions (particularly when done by surgical teams). Our centre’s experience is that meticulous sequential dilation usually allows the skin to stretch to accommodate the cannulas while keeping a tight fit to prevent bleeding and haematoma formation. It is also often faster. The advantage of the open cannulation technique is it can give excellent visualisation and confirmation of the vessels and may decrease vessel wall damage.
Q10. Describe how you will advance the cannula into the patient.
Even after dilation, the lip between the obturator and cannula can get caught at the skin or at the point where the cannula enters the vessel. Twisting (rotating) the cannula upon reaching these points often helps the cannula pass more smoothly.
The cannula should be advanced until all the side holes are beneath the skin and within the vessel. At this point the obturator within the cannula is pulled back to the specified marking before advancing the cannula any further. This is important so that the leading tip of the cannula is the soft plastic at the end of the cannula, not the firm, sharp obturator which can lead to serious or fatal perforations of the right atrium.
The obturator does not need to be pulled back when advancing the shorter arterial cannula at the femoral site for VA ECMO.
Q11. You observe that during femoral-femoral cannulation, both cannulas are in the IVC. Describe how will you position them for VV ECMO?
The IVC is almost always able to accommodate both the access and return cannulas. The access cannula needs to be in more proximal IVC (ie closer to the skin), while the return needs to be distal – usually in the right atrium. In general, a separation of ≥10cm between the distal holes of the access and the return cannulas is needed to prevent recirculation.
We use ultrasound to guide their positioning, usually via a transthoracic subcostal view of the IVC, or a bicaval view during transoesophageal echocardiography (TOE).
Other methods include using an imaging intensifier in radiology or the cath lab, or by measuring the cannula depth at the skin (followed usually by an abdominal or chest X-ray).
Note the last 4cm of the Biomedius single stage cannula tip is plastic – this cannot be seen on X-ray and may appear much lower than it really is. This plastic tip can only be seen with good quality US imaging (e.g. TOE).
Q12. What is the role of the Avalon cannula? What are the pros and cons in this case?
The Avalon cannula combines both access and return cannulas into a single cannula. They are usually larger cannulas (up to 31 Fr), and are typically sited via the internal jugular vein in the neck.
Advantages include the need for only a single puncture and they may be better tolerated enabling mobilisation and rehabilitation.
Disadvantages are that they can be more challenging to position correctly and blood flows may be lower than other dual cannula techniques. Careful positioning is paramount as the returning jet of blood must be directed through the tricuspid valve. Any malposition will lead to recirculation.
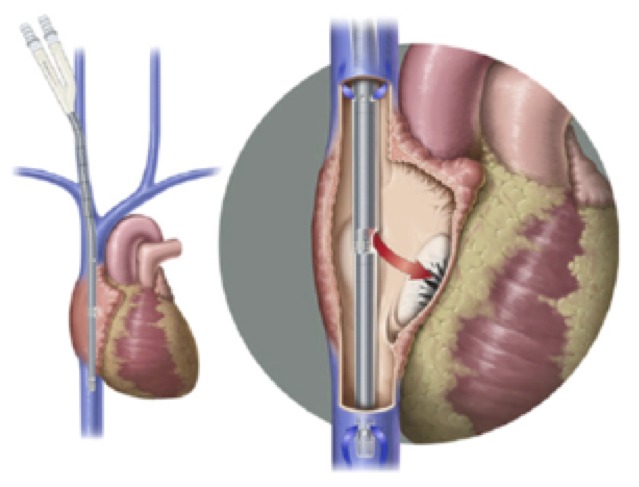
Figure 8. Avalon ECMO cannula. From: Lazar DA, et al. (2012) Journal of Pediatric Surgery 47(2):430-4 (Click image for source)
References and Links
- Pellegrino V, Ihle J, Hilton A, Murphy D. Guideline for Cannulation for Peripheral ECMO. Alfred ICU, 2012
If you want to learn ECMO cannulation come to the Alfred ICU ECMO Cannulation course. It is held twice yearly — details are available at the Alfred ICU Courses website.
Pingback: Keep calm and cannulate! – Global Intensive Care
It should be Nitric oxide , not nitrous oxide
Thanks for spotting the typo!
Chris
Less recirculation with Femoral drainage and RIJ return compared with Fem-Fem set up surely?
Agree easier to transport in fem fem configuration though.
Grant Price, Edinburgh
with fem-IJ, the returning oxygenated blood (IJ cannula) is flowing towards the drainage cannula, increasing the risk of recirc…vs a fem-fem config where the oxygenated blood is flowing away from the drainage cannula.