Author: Steve Musca
Peer reviewers: Arne Diehl, Chris Nickson
Everything ECMO 029
You are working night shift and take handover of a 30-year-old female who has had a bilateral sequential lung transplant for pulmonary arterial hypertension. She returned from the operating theatre on peripheral V-A ECMO as planned pre-operatively. There were no reported problems with the lung transplant or the ECMO.
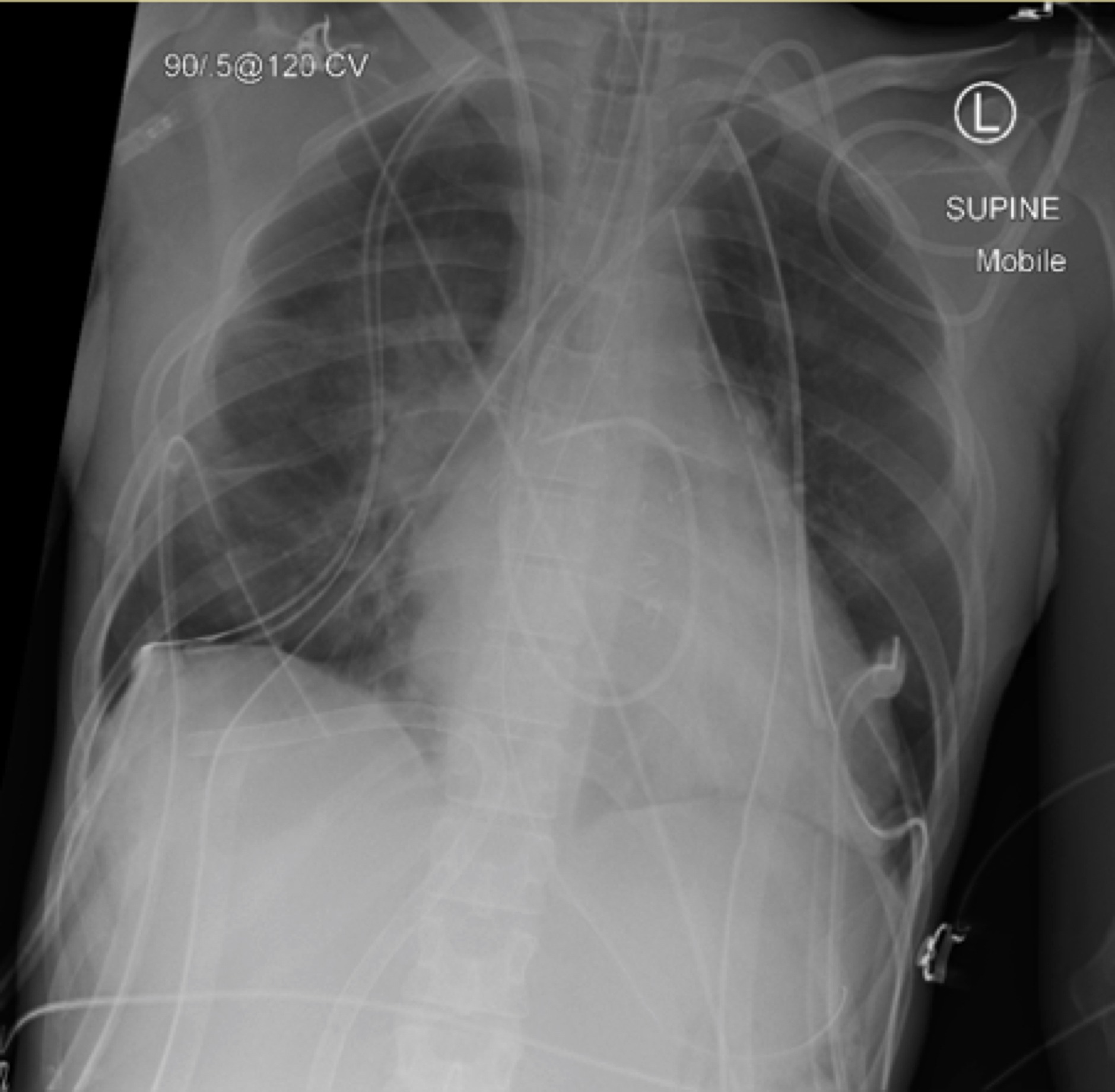
The first post-operative chest x-ray has just been performed:
Q1. Interpret the chest x-ray shown above.
Lines and tubes:
- The ECMO access cannula is passing up the inferior vena cava (IVC) and veering deep into a hepatic vein.
- Endotracheal tube (ETT), nasogastric tube, central line and pulmonary artery catheter (PAC) are all appropriately positioned.
- 6 drains (basal and apical ICCs bilaterally and 2 mediastinal drains).
Heart and lungs:
- Multiple surgical clips seen
- Crowded bi-hilar regions in keeping with severe pulmonary hypertension.
- Probable residual left pneumothorax
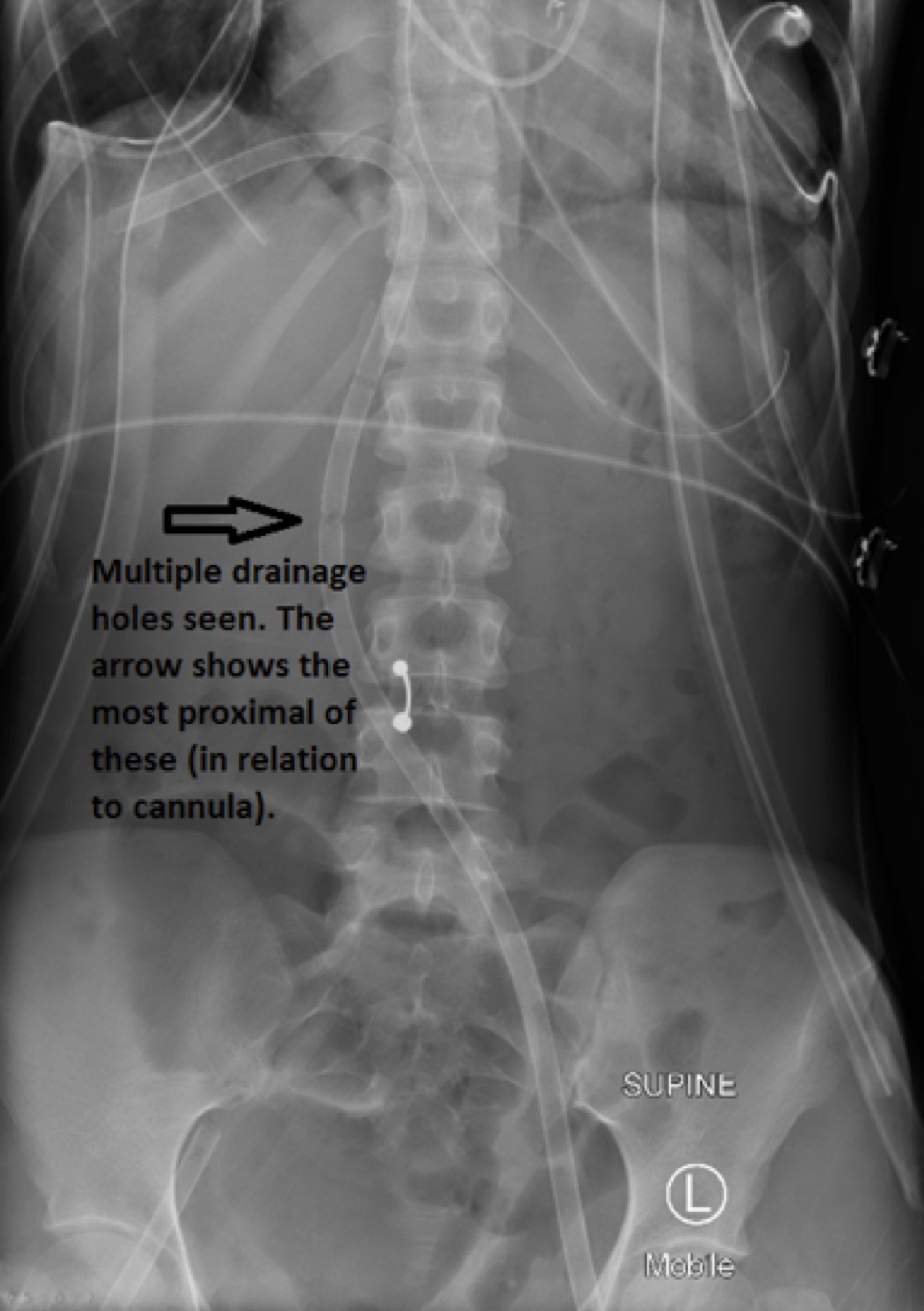
Q2. The ECMO circuit seems to run without signs of access insufficiency despite the cannula position. How is that possible? Take a close look at the abdominal x-ray below.
The abdominal plain film shows that this is a ‘multi-stage’ access cannula with multiple drainage holes in the cannula up to 20cm from the tip. Even if the tip of the cannula is unable to tolerate much inflow in this situation, the main drainage will occur at the proximal openings along the IVC. The pressure gradient across the cannula is also largest at the most proximal openings. Access insufficiency, therefore, may not occur.
The return cannula is also seen, inserted in the right common femoral artery.
Q3. How would you go about retracting the access cannula?
It would be disastrous if pulled back too far with the proximal drainage hole in an extravascular position. As if an opening exits the vessel, significant air would be entrained into the circuit through the negative pressure access limb. The abdominal film, however, is reassuring as the drainage holes finish 20cm from the tip of the cannula and there is a long intravascular passage before leaving the femoral vein.
It is best retracted under strict asepsis (1st operator) and echocardiographic guidance (2nd operator) to capture the cannula tip being withdrawn into the IVC. The ECMO blood flow may temporarily be reduced to avoid negative pressure at the end of the cannula (3rd operator).
Q4. Whilst getting ready for retraction, you look up at the monitor and see the following. What is your observation and what do you think is going on?
- There is almost complete loss of pulsatility seen on the arterial line, as well as the PA/CVP/pulse oximetry traces. Sinus rhythm is preserved.
- The end tidal CO2 is very low, indicating low pulmonary perfusion from low intrinsic cardiac output.
- Given the maintained ECMO flow and MAP you are concerned about cardiac tamponade or an intra-cardiac flow obstruction. The patient needs an echo urgently!
Q5. You perform a TTE using the subcostal window. Interpret the findings.
- There is a large pericardial effusion suggesting haemopericardium.
- The right ventricular wall appears thickened and almost completely collapsed (in keeping with tamponade physiology).
- A D-shaped left ventricle in the short axis view is also seen in cardiac tamponade.
Q5.
You phone the cardiothoracic surgeons to arrange an urgent re-sternotomy. Given theatre won’t be ready for another hour and you are concerned about losing adequate access pressure with the current placement of the access cannula, you re-position as described earlier.
Describe the before and after subcostal echo images.
“Before” image:
“After” image:
“Before” image
- the access cannula is seen diverted down a hepatic vein (towards 8’oclock). Its path up the IVC (10 o’clock) is not visible in this slice.
“After” image
- The access cannula is retracted just below the IVC/RA junction. Colour flow doppler confirms this is the tip of the cannula.
The patient returns from the operating theatre after decompression of the pericardial effusion with a complete return of pulsatility and is on the road to recovery.
Great work!