Author: Tom Rozen
Peer reviewer: Lloyd Roberts
A 40 year old man presents with near syncopal events and has low oxygen saturations in the emergency department, on a past history of systemic hypertension. His blood pressure is low-normal and the chest X ray is clear, so he goes on to have an urgent CTPA which shows bilateral PE with a large burden of clot in both the left and right main pulmonary artery. Low dose thrombolysis is considered to minimise the risk of long term pulmonary hypertension. The patient is transferred to ICU and an urgent echo is performed to assess the right ventricle.
Here are the first loops, can you spot any subtle pathology on these initial scans?
A bit about the RV in PE:
The right ventricle drapes around the LV. In response to an acute Pulmonary Embolus (PE) it first dilates. The RV can’t generate much force without training, so when the Pulmonary Vascular Resistance (PVR) first rises with a PE, the pulmonary artery pressures don’t actually rise substantially because the RV can’t generate large pressures.
Looking at the ventricle in short axis, the septum may bow towards the LV which will form a D shape in diastole, producing a “volume overloaded right ventricle” appearance.
Only later when the RV has been trained will it be able to generate higher pressures. If the LV is D shaped in systole, this is a “pressure overloaded right ventricle”.
Acute cor pulmonale with both pressure AND volume overload (D shape in systole AND diastole) is often absent.
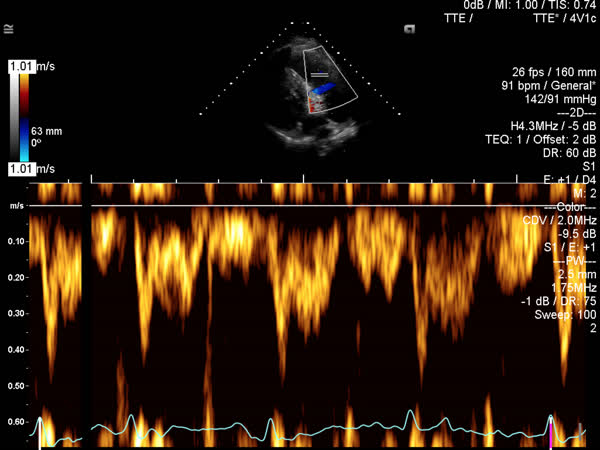
What do you make of the PW doppler through the RVOT in the parasternal short axis view:
What is going on with the right ventricle here?
Do you know what McConnell’s sign is?
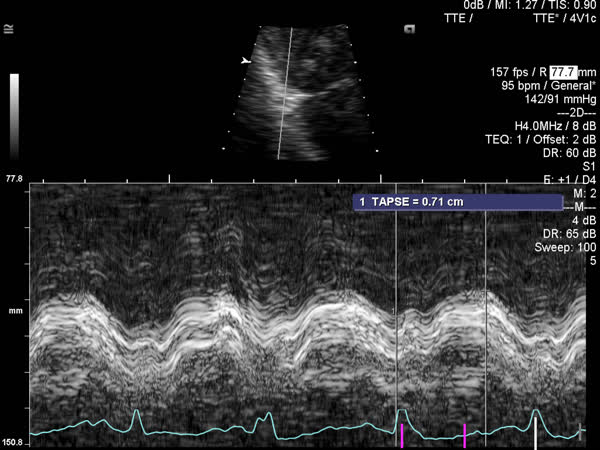
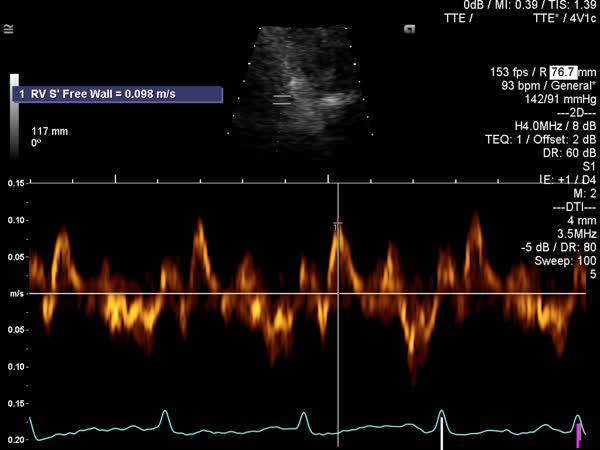
Can we make a quantitative assessment of RV function?
What is this?
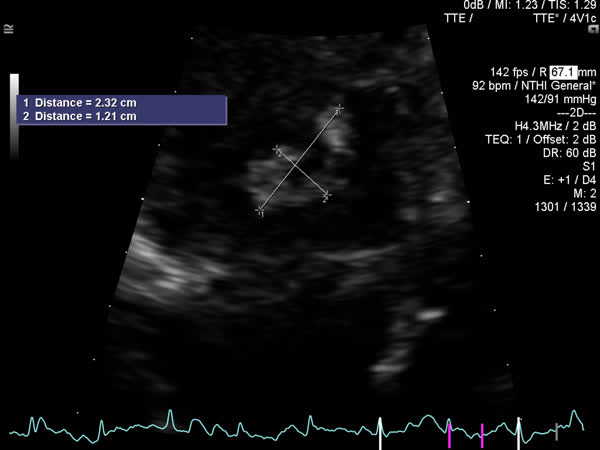
Dimensions of visualised thrombus: 2.3cm x 1.2cm
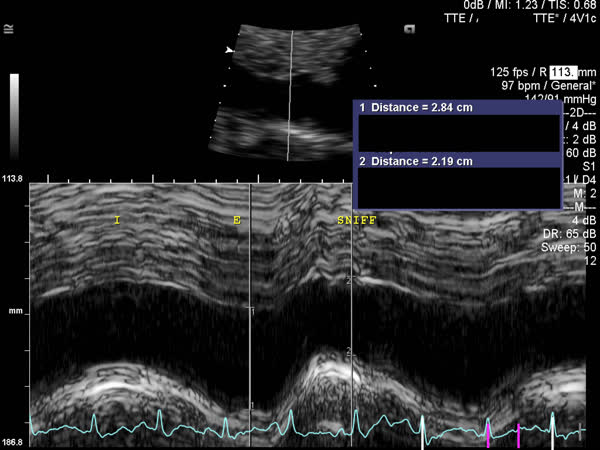
In the non-intubated patient, how does IVC size correlate with CVP?
For simplicity and uniformity of reporting, ASE/EAE recommends:
- IVC diameter <2.1cm that collapses >50% with a sniff suggests normal RA pressure of 3 mmHg (range, 0-5 mmHg).
- IVC diameter >2.1cm that collapses <50% with a sniff suggests high RA pressure of 15 mmHg (range, 10-20 mmHg).
- If IVC diameter and collapse do not fit this paradigm, an intermediate value of 8 mmHg (range, 5-10 mmHg) may be used.
Note, this is in the spontaneously breathing, non-intubated patient.
So what happened here?
- Heparin was continued at a therapeutic range.
- Discussion with cardiac surgeons and radiology regarding clot extraction.
- The patient proceeded to angiographically-directed thrombolysis and clot aspiration
- DVT study was performed demonstrating further clot burden in the legs
- An IVC filter was placed
References:
- ASE Guidelines for the Echocardiographic Assessment of the Right Heart in Adults, Rudski et al 2010
- ASE Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults, Lang et al 2015
- BSE Guidelines for Chamber Quantification, Masani et al 2011
- Textbook of Clinical Echocardiography, Otto 2013
- Non Invasive Haemodynamics at Rest, escardio.org 2010
- Life in the Fast Lane: Thrombolysis for submassive pulmonary embolus, Nickson 2014
- ASE’s Comprehensive Echocardiography, Chapter 37 (Pulmonary embolism), Zhao et al 2015
- Kurzyna, M., Torbicki, A., Pruszczyk, P., Burakowska, B., Fijałkowska, A., Kober, J., et al. (2002). Disturbed right ventricular ejection pattern as a new Doppler echocardiographic sign of acute pulmonary embolism. The American Journal of Cardiology, 90(5), 507–511.
Simultaneously published on Echopraxis.com