Labs and Lytes 029
Author: Eamon Raith
Reviewers: Sarah Yong, Chris Nickson
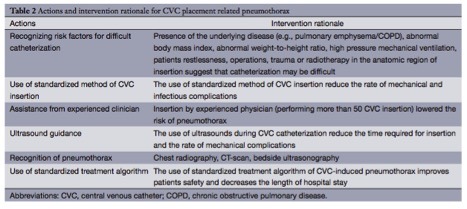
A 50-year-old man is admitted to ICU postoperatively, following a ‘pedestrian versus car’ motor vehicle accident. He requires ongoing haemodynamic support with noradrenaline. A left subclavian CVC is inserted with dynamic ultrasound guidance.
Click image to enlarge
Q1. Describe and interpret the chest radiograph (CXR)
A systematic approach to the assessment of the chest radiograph is required. A simple structure takes the following approach:
- Summary
- Technical aspects
- Lungs & pleural cavity
- Heart & mediastinum
- Bones
- Soft tissues
- Indwelling devices
This is an AP film of a supine patient. The most striking finding is the presence of extensive ‘hardware’:
- L) subclavian and R) IJ central lines, tips appropriately placed
- Endotracheal tube
- Thoracic spinal fixation
- Thoracic aortic stent
- Surgical staples
- ECG leads
Additionally:
Technical aspects:
- Film is minimally rotated, adequately exposed
- All aspects of interest are located within the field
Lungs and pleural cavity:
- Prominent horizontal fissure (right)
- Mild alveolar opacification in the left lower lobe, consistent with possible pulmonary contusion, given the mechanism of injury
Heart and mediastinum:
- Cardiothoracic ratio is ~50%, although that can be accounted for by the AP projection
- Right and left mediastinal contours appear normal
- Thoracic aortic stent, extending to the level of the left subclavian artery
Bones:
- Bilateral rib fractures
- Thoracic spinal fusion
Soft tissues:
- Normal diaphragmatic outlines
- Absence of deep sulcus sign
The patient has a weak left radial artery pulse, and it is suspected that the aortic stent has compromised distal flow to the left arm. A CT aortogram is ordered.
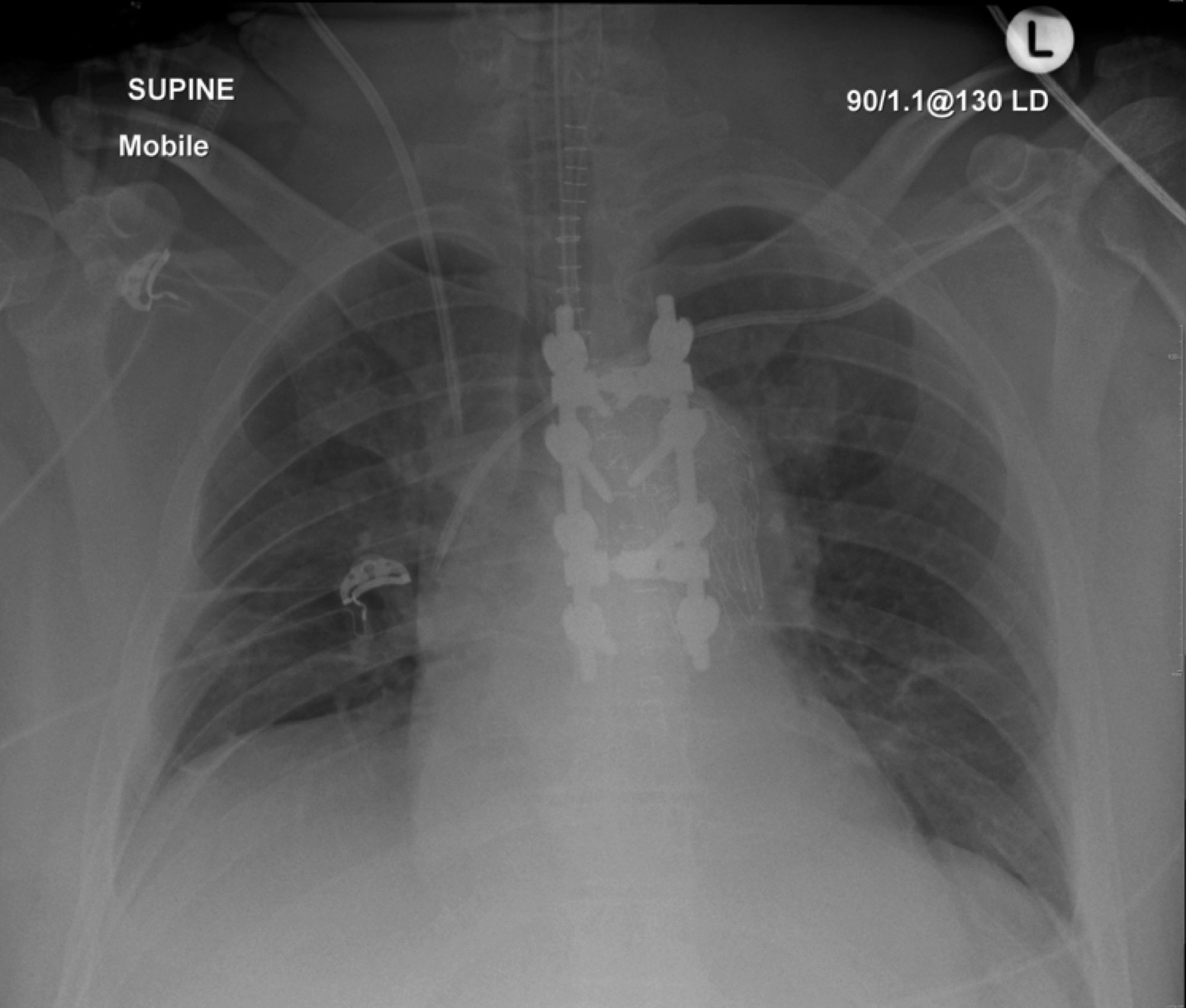
Q2. Describe and interpret the pilot image shown below.
Click image to enlarge
The most striking finding is the presence of a ‘deep sulcus sign’ on the left, with hyperlucency and absence of lung markings, consistent with a left pneumothorax.
Other findings include:
- Left rib fractures
- Possible tracheal deviation to the right (difficult to determine given the presence of metalwork and the patient’s positioning)
- Hardware: ETT, L) internal jugular CVC, thoracic spinal fusion, pelvic external fixation and ECG leads
Q3. What is the ‘deep sulcus’ sign?
The deep sulcus sign is an indirect sign of a pneumothorax, found on supine chest radiographs. It is caused by the non-dependent distribution of intrapleural air, producing abnormal anterior diaphragmatic lucency, and thus a deepening of the costophrenic angle, as air tracks latero-caudally.2
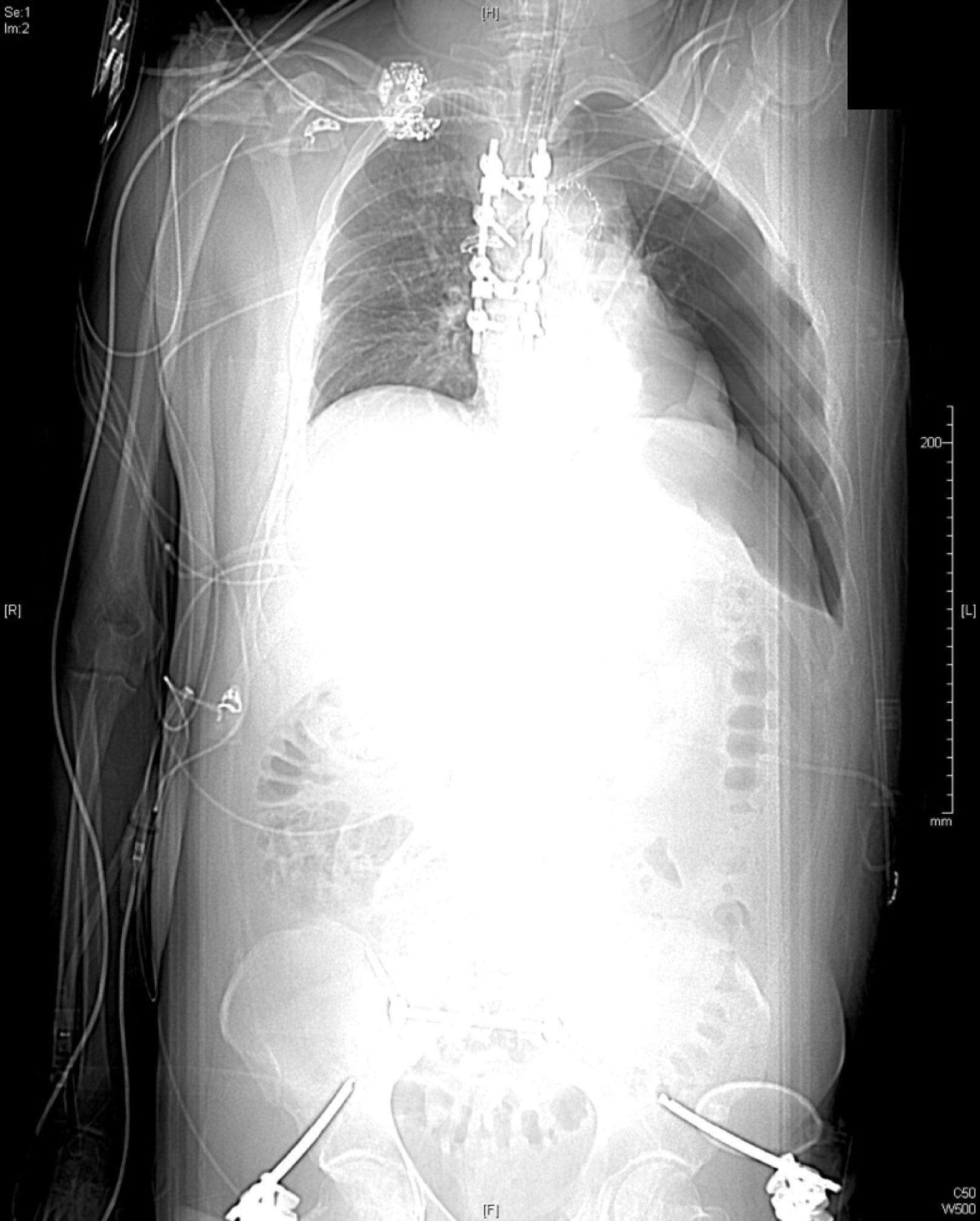
Q4. How common is pneumothorax post CVC insertion? How can this risk be minimised?
Pneumothorax is a common complication of CVC insertion, representing up to 30% of mechanical adverse events. The likelihood of mechanical complications is largely determined by three categories of factors;1
- Patient-related factors (underlying disease, co-morbidity, anatomy, compromised procedural settings, patient restlessness or lack of co-operation, previous operations/trauma/radiotherapy).
- Catheter-related factors (site, catheter type).
- Clinical factors (Operator experience, previous catheterizations, catheterization attempts, emergency vs. elective situation).
Pneumothorax is the most likely mechanical complication associated with subclavian vein cannulation (see below).1
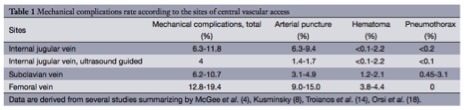
Table from Tsotsolis, N. et al (2015)
CVC-associated pneumothorax can be prevented or rapidly managed through the following:
- Recognition of risk factors for difficult catheterization
- Use of a standard method of CVC insertion
- Assistance from an experienced clinician,
- Use of ultrasound guidance
- Early recognition of the presence of pneumothorax
- Use of a standardized treatment algorithm.
The rationale for each of these interventions is outlined in the table below;1
References and Links
- Tsotsolis N, Tsirgogianni K, Kioumis I. Pneumothorax as a complication of central venous catheter insertion. Annals of translational medicine. 3(3):40. 2015. [pubmed] [free full text]
- Sabbar S, Nilles EJ. Images in clinical medicine. Deep sulcus sign. The New England journal of medicine. 366(6):552. 2012. [pubmed] [free full text]