Labs and Lytes 022
Author: Sarah Yong
Reviewer: Chris Nickson
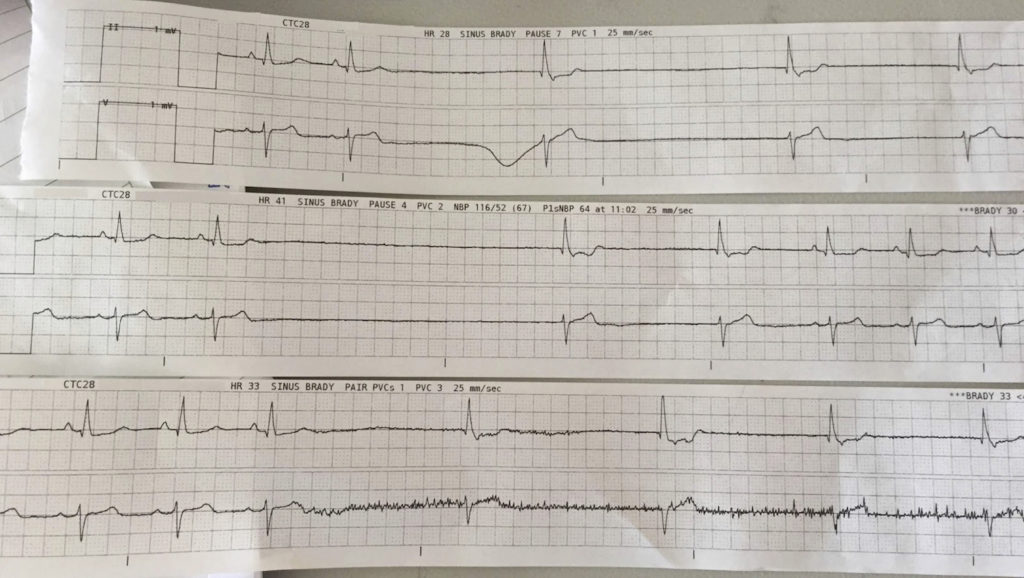
You have just arrived at a MET call for a 73 year-old lady admitted overnight with recurrent falls and collapse for investigation. At first glance the patient is alert and looks comfortable. You hear the monitor alarming constantly as the nurse passes you the following rhythm strips:
Q1. What is your interpretation of these rhythm strips?
Sinus bradycardia HR ~60 bpm with intermittent sinus arrest / sinus exit block, shown by 2 missing p waves followed by 2 ventricular escape beats at a rate just under 40 bpm
Q2. What would you like to do next?
- Assess the patient
- Decide if they’re stable or unstable
- Look for underlying cause
Assess the patient
- Assess ABCDE
- Simultaneously apply monitoring (SpO2, ECG, NIBP) and O2 if required
Are they stable, unstable or have high-risk features?
- This will help determine your next steps in management
- Patients are considered “unstable” if there are features of myocardial ischaemia, shock, acute heart failure or hypotension
- Patients are high risk for asystole if they have had recent asystole, complete heart block with broad QRS, Mobitz II AV block or ventricular pauses > 3 seconds
- If they’re unstable or have high risk features, give atropine 500-600mcg IV and prepare for pacing (see below)
Look for an underlying cause (see the LITFL Bradycardia DDX page for the differentials)
- 12 lead ECG: myocardial ischaemia, myocarditis, cardiomyopathy
- Transthoracic echo: structural dysfunction
- Bloods: FBE, UEC, CMP, thyroid function
- Rule out infection: septic screen if indicated
- Exclude hypothermia, medications, toxins
On further assessment, the patient remains alert and asymptomatic with no chest pain, shortness of breath or presyncope. HR remains 59 with ongoing pauses of up to 4 seconds and episodes of bradycardia down to 30 bpm. BP was 96/, improving to 127/75 when the rate spontaneously picks up to 60 bpm.
Q3. What management options are available for this condition?
Management includes pacing via pharmacological, transcutaneous, transvenous or epicardial routes.
Pharmacological
- Atropine 500 – 600mcg boluses, repeat to max 3mg
- Adrenaline infusion up to 10mcg/min
- Isoprenaline infusion 0.5 – 5mcg/min
Transcutaneous
- Temporary cardiac pacing via defibrillator using pads or paddles placed externally on chest
Transvenous
- Temporary: bipolar pacing lead (II guidance), paceport PA catheter, or balloon flotation leads
- Permanent: single chamber, dual chamber, bi-ventricular (resynchronisation), pacemaker-defibrillator
Epicardial
- Used in the post-cardiac surgery patient with temporary epicardial AV pacing wires in situ (inserted by surgeon prior to closure)
Q4. The patient is commenced on an isoprenaline infusion at 0.5mcg/min, with improvement in his rhythm. Briefly describe the mechanism of action and potential adverse effects of this drug
Isoprenaline is a synthetic sympathomimetic drug with almost exclusive beta agonist effects. Isoprenaline is called isoproterenol in North America.
It can be administered via a proximal peripheral line in the short term, so it is worthwhile preparing it before the patient becomes unstable. Low-dose isoprenaline infusion can be run on the cardiac wards at The Alfred.
Potential adverse effects include:
- Worsening cardiac function: by increasing myocardial oxygen demand while decreasing effective coronary perfusion
- Ventricular arrhythmias
- Worsening of heart block
- Contains sulfite moiety: potential allergic / anaphylactic reaction
References and links
- LITFL — Bradycardia Differential Diagnosis
- LITFL ECG Library — Sinoatrial exit block
- LITFL CCC — Transcutaneous pacing
- LITFL CCC — Temporary transvenous cardiac pacing
- LITFL Critical Care Drug Handbook — Isoprenaline
- Resus.org.uk — Bradyarrhythmia algorithm